Sunday Poster Session
Category: Colorectal Cancer Prevention
P0430 - Impact of Colonoscopy Difficulty on Adenoma Detection Rate and Adenomas Per Colonoscopy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Brian R. Hughes, MD
University of Colorado Anschutz Medical Campus
Aurora, CO
Presenting Author(s)
Brian R. Hughes, MD1, Swati G. Patel, MD, MS2, Blake Jones, MD3
1University of Colorado Anschutz Medical Campus, Aurora, CO; 2University of Colorado School of Medicine and Rocky Mountain VA Regional Medical Center, Aurora, CO; 3Endeavor Health, Chicago, IL
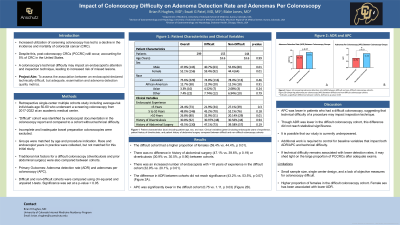
Introduction: Post-colonoscopy colorectal cancer (PCCRC) accounts for 5% of CRC in the United States, with the majority being attributed to missed lesions in adequate examinations. Endoscopist attention and inspection technique may be impacted by the technical difficulty of a procedure. Our aim was to assess the association between an endoscopist-declared technically difficult, but adequate, examination and adenoma detection quality metrics.
Methods: This was a retrospective single-center multiple cohorts study including average-risk individuals age 50-60 who underwent a screening colonoscopy from 2017-2022 at an academic medical center. The “difficult” cohort was identified by endoscopist documentation in the colonoscopy report and compared to a cohort without technical difficulty. Incomplete and inadequate bowel preparation colonoscopies were excluded. Patient demographics and clinical data were abstracted. Groups were matched by age and procedure indication. Race and endoscopist years in practice were collected, but not matched for this initial study. Traditional risk factors for a difficult colonoscopy (diverticulosis and prior abdominal surgery) were also compared. Outcomes included adenoma detection rate (ADR) and adenomas per colonoscopy (APC). Difficult and non-difficult cohorts were compared using chi-squared and unpaired t-tests. Significance was set at a p-value < 0.05.
Results: 299 colonoscopies were included; 155 difficult, 144 non-difficult, the average age was 53.6 years in both groups. The difficult cohort had a higher proportion of females (59.4% vs. 44.4%, p 0.01). Race did not differ between cohorts. There was no difference in history of abdominal surgery (47.1% vs. 39.6%, p 0.19) or diverticulosis (30.9% vs. 30.5%, p 0.90). There was an increased number of endoscopists with >10 years of experience in the difficult cohort (32.9% vs. 20.1%, p 0.01). The difference in ADR between cohorts did not reach significance (43.2% vs. 53.5%, p 0.07). APC was significantly lower in the difficult cohort (0.75 vs. 1.11, p 0.03). A summary of the results can be found in Table 1.
Discussion: APC was lower in patients who had a difficult colonoscopy, suggesting that technical difficulty of a procedure may impact inspection technique. Additional work is required to control for baseline variables that impact both ADR/APC and technical difficulty. If technical difficulty remains associated with lower detection rates, it may shed light on the large proportion of PCCRCs after adequate exams.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Brian R. Hughes, MD1, Swati G. Patel, MD, MS2, Blake Jones, MD3. P0430 - Impact of Colonoscopy Difficulty on Adenoma Detection Rate and Adenomas Per Colonoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Colorado Anschutz Medical Campus, Aurora, CO; 2University of Colorado School of Medicine and Rocky Mountain VA Regional Medical Center, Aurora, CO; 3Endeavor Health, Chicago, IL
Introduction: Post-colonoscopy colorectal cancer (PCCRC) accounts for 5% of CRC in the United States, with the majority being attributed to missed lesions in adequate examinations. Endoscopist attention and inspection technique may be impacted by the technical difficulty of a procedure. Our aim was to assess the association between an endoscopist-declared technically difficult, but adequate, examination and adenoma detection quality metrics.
Methods: This was a retrospective single-center multiple cohorts study including average-risk individuals age 50-60 who underwent a screening colonoscopy from 2017-2022 at an academic medical center. The “difficult” cohort was identified by endoscopist documentation in the colonoscopy report and compared to a cohort without technical difficulty. Incomplete and inadequate bowel preparation colonoscopies were excluded. Patient demographics and clinical data were abstracted. Groups were matched by age and procedure indication. Race and endoscopist years in practice were collected, but not matched for this initial study. Traditional risk factors for a difficult colonoscopy (diverticulosis and prior abdominal surgery) were also compared. Outcomes included adenoma detection rate (ADR) and adenomas per colonoscopy (APC). Difficult and non-difficult cohorts were compared using chi-squared and unpaired t-tests. Significance was set at a p-value < 0.05.
Results: 299 colonoscopies were included; 155 difficult, 144 non-difficult, the average age was 53.6 years in both groups. The difficult cohort had a higher proportion of females (59.4% vs. 44.4%, p 0.01). Race did not differ between cohorts. There was no difference in history of abdominal surgery (47.1% vs. 39.6%, p 0.19) or diverticulosis (30.9% vs. 30.5%, p 0.90). There was an increased number of endoscopists with >10 years of experience in the difficult cohort (32.9% vs. 20.1%, p 0.01). The difference in ADR between cohorts did not reach significance (43.2% vs. 53.5%, p 0.07). APC was significantly lower in the difficult cohort (0.75 vs. 1.11, p 0.03). A summary of the results can be found in Table 1.
Discussion: APC was lower in patients who had a difficult colonoscopy, suggesting that technical difficulty of a procedure may impact inspection technique. Additional work is required to control for baseline variables that impact both ADR/APC and technical difficulty. If technical difficulty remains associated with lower detection rates, it may shed light on the large proportion of PCCRCs after adequate exams.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Brian Hughes indicated no relevant financial relationships.
Swati Patel: Olympus America – Grant/Research Support.
Blake Jones indicated no relevant financial relationships.
Brian R. Hughes, MD1, Swati G. Patel, MD, MS2, Blake Jones, MD3. P0430 - Impact of Colonoscopy Difficulty on Adenoma Detection Rate and Adenomas Per Colonoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
