Sunday Poster Session
Category: Colorectal Cancer Prevention
P0433 - Impact of COVID-19 on Colorectal Screening Rates in the San Diego Population
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Isabelle Nguyen, MD
Scripps Health
La Jolla, CA
Presenting Author(s)
Isabelle Nguyen, MD1, Jennifer Hou, MD, PhD1, Leah Puglisi, MS2, Franklin Tsai, MD1
1Scripps Green Hospital, La Jolla, CA; 2Scripps Research, La Jolla, CA
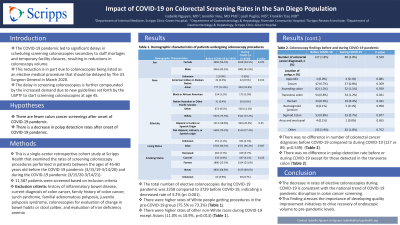
Introduction: The COVID-19 pandemic caused numerous disruptions to routine healthcare maintenance. Specifically, there have been significant delays in scheduling screening colonoscopies secondary to staff shortages and temporary facility closures, resulting in reductions in colonoscopy volume. This reduction is in part due to colonoscopies being listed as an elective medical procedure that should be delayed by The US Surgeon General in March 2020. The delay in screening colonoscopies is further compounded by the increased demand due to new guidelines set forth by the USPTF to start screening colonoscopies at age 45 (previously at age 50). Based on a predictive model of current trends in colonoscopy and breast cancer screenings, it is anticipated that the incidence of colorectal cancer (CRC) may experience an upward trajectory over the next decade.
Methods: This single-center retrospective cohort study examined the rates of screening colonoscopy procedures performed in patients between the ages of 45-80 years old during the 1-year interval before the pandemic (March 15, 2019-March 14, 2020) and during the pandemic (March 15, 2020-March 14, 2021). 11,587 patients were screened based on inclusion criteria and were excluded based on history of inflammatory bowel disease, family history of colon cancer, Lynch syndrome, familial adenomatous polyposis, juvenile polyposis syndrome, colonoscopies for evaluation of change in bowel habits or stool caliber, and evaluation of iron deficiency anemia.
Results: The total number of elective colonoscopies during COVID was 2258 compared to 3729 before COVID, indicating a decreased rate of 3.2% (p< 0.001). In a subgroup analysis, there were higher rates of White people getting procedures in the pre-COVID group (75.5% vs 73.2%) and there were higher rates of other non-White races in the post-COVID group (11.1% vs 9.5%, p=0.013). There was no difference in number of colorectal cancer diagnoses before COVID compared to during COVID (127 vs 89, p=0.539). In addition, there was no difference in polyp detection rate before or during COVID except for those detected in the transverse colon (Table 1).
Discussion: The decrease in rates of elective colonoscopies during COVID-19 is consistent with the national trend of COVID-19 pandemic disruption in colon cancer screening. This finding stresses the importance of developing quality improvement initiatives to drive recovery of endoscopic volume to pre-pandemic levels.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Isabelle Nguyen, MD1, Jennifer Hou, MD, PhD1, Leah Puglisi, MS2, Franklin Tsai, MD1. P0433 - Impact of COVID-19 on Colorectal Screening Rates in the San Diego Population, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Scripps Green Hospital, La Jolla, CA; 2Scripps Research, La Jolla, CA
Introduction: The COVID-19 pandemic caused numerous disruptions to routine healthcare maintenance. Specifically, there have been significant delays in scheduling screening colonoscopies secondary to staff shortages and temporary facility closures, resulting in reductions in colonoscopy volume. This reduction is in part due to colonoscopies being listed as an elective medical procedure that should be delayed by The US Surgeon General in March 2020. The delay in screening colonoscopies is further compounded by the increased demand due to new guidelines set forth by the USPTF to start screening colonoscopies at age 45 (previously at age 50). Based on a predictive model of current trends in colonoscopy and breast cancer screenings, it is anticipated that the incidence of colorectal cancer (CRC) may experience an upward trajectory over the next decade.
Methods: This single-center retrospective cohort study examined the rates of screening colonoscopy procedures performed in patients between the ages of 45-80 years old during the 1-year interval before the pandemic (March 15, 2019-March 14, 2020) and during the pandemic (March 15, 2020-March 14, 2021). 11,587 patients were screened based on inclusion criteria and were excluded based on history of inflammatory bowel disease, family history of colon cancer, Lynch syndrome, familial adenomatous polyposis, juvenile polyposis syndrome, colonoscopies for evaluation of change in bowel habits or stool caliber, and evaluation of iron deficiency anemia.
Results: The total number of elective colonoscopies during COVID was 2258 compared to 3729 before COVID, indicating a decreased rate of 3.2% (p< 0.001). In a subgroup analysis, there were higher rates of White people getting procedures in the pre-COVID group (75.5% vs 73.2%) and there were higher rates of other non-White races in the post-COVID group (11.1% vs 9.5%, p=0.013). There was no difference in number of colorectal cancer diagnoses before COVID compared to during COVID (127 vs 89, p=0.539). In addition, there was no difference in polyp detection rate before or during COVID except for those detected in the transverse colon (Table 1).
Discussion: The decrease in rates of elective colonoscopies during COVID-19 is consistent with the national trend of COVID-19 pandemic disruption in colon cancer screening. This finding stresses the importance of developing quality improvement initiatives to drive recovery of endoscopic volume to pre-pandemic levels.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Isabelle Nguyen indicated no relevant financial relationships.
Jennifer Hou indicated no relevant financial relationships.
Leah Puglisi indicated no relevant financial relationships.
Franklin Tsai indicated no relevant financial relationships.
Isabelle Nguyen, MD1, Jennifer Hou, MD, PhD1, Leah Puglisi, MS2, Franklin Tsai, MD1. P0433 - Impact of COVID-19 on Colorectal Screening Rates in the San Diego Population, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
