Sunday Poster Session
Category: Esophagus
P0481 - Radiofrequency Ablation and Cryoablation for Dysplastic Barrett's Esophagus: A Potential Cause of Esophageal Mucosal Eosinophilia
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E


Sidra Naz, MD, MPH
University of Texas MD Anderson Cancer Center
Houston, TX
Presenting Author(s)
Sidra Naz, MD, MPH1, Phillip Lum, BS2, Marta Davila, MD3, Deyali Chatterjee, MD3, Jianliang Dai, PhD2, George Triadafilopoulos, MD4, Mehnaz A. Shafi, MD1
1University of Texas MD Anderson Cancer Center, Houston, TX; 2MD Anderson Cancer Center, Houston, TX; 3The University of Texas MD Anderson Cancer Center, Houston, TX; 4Stanford University School of Medicine, Houston, TX
Introduction: Esophageal mucosal eosinophilia (EME) is commonly associated with gastroesophageal reflux disease (GERD) or eosinophilic esophagitis (EoE), but it could also result from ablation-induced non-specific injury.To retrospectively review the clinical, endoscopic, and histological findings of patients who developed EME after radiofrequency ablation (RFA) therapy or cryoballoon ablation (CBA) for dysplastic Barrett's esophagus (BE).
Methods: We examined the clinical, endoscopic, and histological findings of all patients with both HGD or LGD dysplastic BE who underwent endoscopic RFA and/or CBA therapy between February 2010 and February 2024 to identify EME on post-RFA and post-CBA biopsies. Patients with preexisting EoE prior to therapy were excluded. All pathology slides were systematically reviewed for the maximum number of eosinophils per high-power field (hpf). Risk factors for EME, dysphagia, and the use of proton pump inhibitors (PPI) were reviewed. The esophageal endoscopic appearance post-ablation in these patients was evaluated for stricture(s), ulcers, exudates, or EoE-like features. We also studied the BE length before and after ablation, number of RFA or CBA treatments, time interval to the development of EME post-RFA or CBA, and any subsequent resolution of EME.
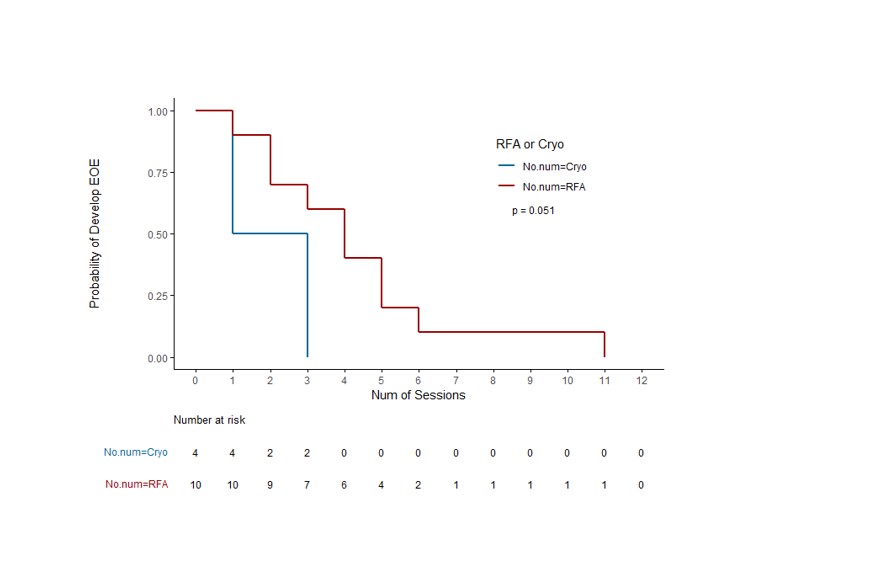
Results: 707 patients underwent RFA +/- CBA for both LGD or HGD dysplastic BE and had post-treatment biopsies. 668 patients underwent RFA alone, an additional 39 patients underwent both RFA and CBA. Fourteen (2%) of patients had EME (eosinophils > 20/hpf). All patients were White; 80% of the RFA and 75% of the RFA + cryoablation group had h/o seasonal allergies. PPI use at the time of post-treatment biopsies was 100% in the RFA and 75% in RFA + CBA group. The median duration of EME was 19.7 months. No significant difference was identified in the covariates between the RFA +/- CBA treatment groups by Fisher's exact or Wilcoxon rank sum tests. However, Kaplan-Meier (KM) curve analyses analysis of the number of treatment sessions using RFA +/- CBA showed borderline significant difference in the development of EME (log-rank test p=0.051)
Discussion: The development of new onset EME after RFA +/- CBA for dysplastic BE was seen in 2% of our cohort; 80% patients had seasonal allergies. Dysphagia was rare. EME persisted for >19 months. EME eradication rates using acid suppression and/or topical steroids were 50% in both cohorts. EME, seems distinct from EoE and is probably a consequence of RFA and CBA therapy.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sidra Naz, MD, MPH1, Phillip Lum, BS2, Marta Davila, MD3, Deyali Chatterjee, MD3, Jianliang Dai, PhD2, George Triadafilopoulos, MD4, Mehnaz A. Shafi, MD1. P0481 - Radiofrequency Ablation and Cryoablation for Dysplastic Barrett's Esophagus: A Potential Cause of Esophageal Mucosal Eosinophilia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas MD Anderson Cancer Center, Houston, TX; 2MD Anderson Cancer Center, Houston, TX; 3The University of Texas MD Anderson Cancer Center, Houston, TX; 4Stanford University School of Medicine, Houston, TX
Introduction: Esophageal mucosal eosinophilia (EME) is commonly associated with gastroesophageal reflux disease (GERD) or eosinophilic esophagitis (EoE), but it could also result from ablation-induced non-specific injury.To retrospectively review the clinical, endoscopic, and histological findings of patients who developed EME after radiofrequency ablation (RFA) therapy or cryoballoon ablation (CBA) for dysplastic Barrett's esophagus (BE).
Methods: We examined the clinical, endoscopic, and histological findings of all patients with both HGD or LGD dysplastic BE who underwent endoscopic RFA and/or CBA therapy between February 2010 and February 2024 to identify EME on post-RFA and post-CBA biopsies. Patients with preexisting EoE prior to therapy were excluded. All pathology slides were systematically reviewed for the maximum number of eosinophils per high-power field (hpf). Risk factors for EME, dysphagia, and the use of proton pump inhibitors (PPI) were reviewed. The esophageal endoscopic appearance post-ablation in these patients was evaluated for stricture(s), ulcers, exudates, or EoE-like features. We also studied the BE length before and after ablation, number of RFA or CBA treatments, time interval to the development of EME post-RFA or CBA, and any subsequent resolution of EME.
Results: 707 patients underwent RFA +/- CBA for both LGD or HGD dysplastic BE and had post-treatment biopsies. 668 patients underwent RFA alone, an additional 39 patients underwent both RFA and CBA. Fourteen (2%) of patients had EME (eosinophils > 20/hpf). All patients were White; 80% of the RFA and 75% of the RFA + cryoablation group had h/o seasonal allergies. PPI use at the time of post-treatment biopsies was 100% in the RFA and 75% in RFA + CBA group. The median duration of EME was 19.7 months. No significant difference was identified in the covariates between the RFA +/- CBA treatment groups by Fisher's exact or Wilcoxon rank sum tests. However, Kaplan-Meier (KM) curve analyses analysis of the number of treatment sessions using RFA +/- CBA showed borderline significant difference in the development of EME (log-rank test p=0.051)
Discussion: The development of new onset EME after RFA +/- CBA for dysplastic BE was seen in 2% of our cohort; 80% patients had seasonal allergies. Dysphagia was rare. EME persisted for >19 months. EME eradication rates using acid suppression and/or topical steroids were 50% in both cohorts. EME, seems distinct from EoE and is probably a consequence of RFA and CBA therapy.
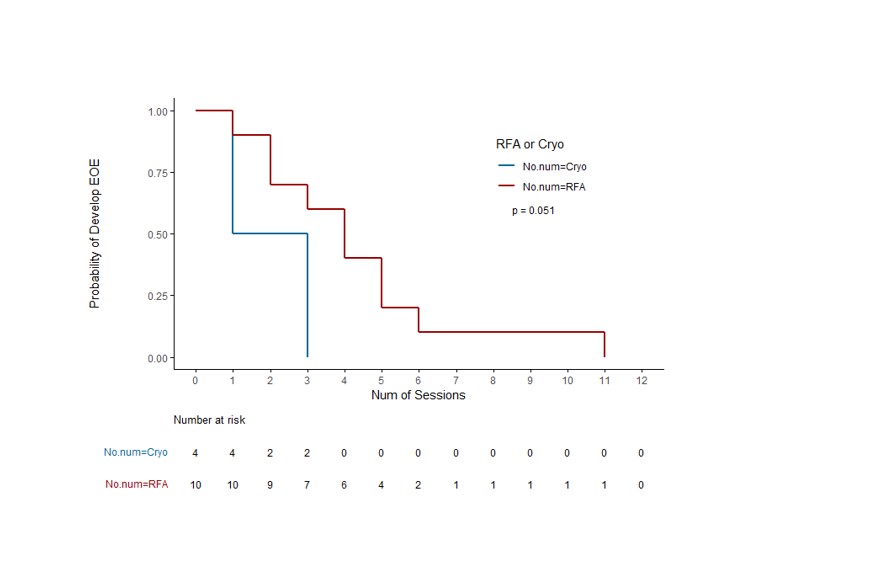
Figure: Fig.1 KM-plots of EME on the number of sessions of RFA +/- CBA treatment.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sidra Naz indicated no relevant financial relationships.
Phillip Lum indicated no relevant financial relationships.
Marta Davila indicated no relevant financial relationships.
Deyali Chatterjee indicated no relevant financial relationships.
Jianliang Dai indicated no relevant financial relationships.
George Triadafilopoulos indicated no relevant financial relationships.
Mehnaz Shafi indicated no relevant financial relationships.
Sidra Naz, MD, MPH1, Phillip Lum, BS2, Marta Davila, MD3, Deyali Chatterjee, MD3, Jianliang Dai, PhD2, George Triadafilopoulos, MD4, Mehnaz A. Shafi, MD1. P0481 - Radiofrequency Ablation and Cryoablation for Dysplastic Barrett's Esophagus: A Potential Cause of Esophageal Mucosal Eosinophilia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
