Sunday Poster Session
Category: Esophagus
P0483 - Bridging Knowledge and Competence Gaps Regarding Recent Therapeutic advances in Eosinophilic Esophagitis: Effectiveness of Continuing Medical Education
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- TA
Tamima Ashraf, PhD
Answers in CME
New York, NY
Presenting Author(s)
Tamima Ashraf, PhD1, Evan S.. Dellon, MD, MPH, FACG2, Meghan Coulehan, MPH1, Emily Kitterman, 1, Aisha Suhail, 1
1Answers in CME, New York, NY; 2University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC
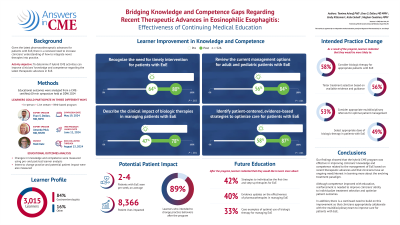
Introduction: Eosinophilic esophagitis (EoE) can considerably impact the quality of life for both children and adults. Given the latest pharmacotherapeutic advances for patients with EoE, there is a renewed need to increase clinicians’ understanding of how to integrate novel therapies into practice. Therefore, we developed a continued medical education (CME) program aimed at improving clinicians’ knowledge and competence related to: recognizing the urgency for timely intervention of EoE; reviewing the current treatment options; describing the impact of biologic therapy; and identifying strategies for evidence-based care.
Methods: A 60-minute CME-certified, interactive symposium titled “Assembling the Puzzle of Eosinophilic Esophagitis: Where Novel Therapies May Fit Into Treatment Plans”, was presented by two gastroenterologists and a patient with EoE at a National GI Conference in spring, 2024. Learners could participate in three different ways- 1) in person, 2) by attending virtually, or 3) by watching the highlights following the live event. Changes in knowledge and competence were measured using pre- and post-test learner analysis. Intent to change practice and potential patient impact were also measured. Data collection is ongoing.
Results: As of June 6, 2024, a total of 266 learners participated, with the leading learner specialties being gastroenterologists (64%). A subset of learners (n=158) completed pre- and post-test assessments. Baseline knowledge was lowest regarding how to optimally utilize biologic therapy in pediatric and adult patients with EoE. Post-education, learners demonstrated a positive change in knowledge/competence related to: impact of delayed diagnosis of EoE (29%); recent therapeutic advances (43%); optimal use of biologic therapies (56%); and evidence-based, multidisciplinary strategies to improve patient care (42%). Of the learners, 96% intended to make changes to their practice based on the activity. Based on learners’ self-report of the number of patients seen per week, this program potentially impacted 796 patient interactions. Nearly half (46%) of learners also expressed interest in receiving further education related to tailoring the selection of first-line and step-up therapies.
Discussion: Our findings showed that i) hybrid CME was effective in improving knowledge and competence among clinicians related to the management of EoE based on recent therapeutic advances, and ii) an ongoing need/interest among clinicians to learn more about the evolving treatment paradigm.
Disclosures:
Tamima Ashraf, PhD1, Evan S.. Dellon, MD, MPH, FACG2, Meghan Coulehan, MPH1, Emily Kitterman, 1, Aisha Suhail, 1. P0483 - Bridging Knowledge and Competence Gaps Regarding Recent Therapeutic advances in Eosinophilic Esophagitis: Effectiveness of Continuing Medical Education, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Answers in CME, New York, NY; 2University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC
Introduction: Eosinophilic esophagitis (EoE) can considerably impact the quality of life for both children and adults. Given the latest pharmacotherapeutic advances for patients with EoE, there is a renewed need to increase clinicians’ understanding of how to integrate novel therapies into practice. Therefore, we developed a continued medical education (CME) program aimed at improving clinicians’ knowledge and competence related to: recognizing the urgency for timely intervention of EoE; reviewing the current treatment options; describing the impact of biologic therapy; and identifying strategies for evidence-based care.
Methods: A 60-minute CME-certified, interactive symposium titled “Assembling the Puzzle of Eosinophilic Esophagitis: Where Novel Therapies May Fit Into Treatment Plans”, was presented by two gastroenterologists and a patient with EoE at a National GI Conference in spring, 2024. Learners could participate in three different ways- 1) in person, 2) by attending virtually, or 3) by watching the highlights following the live event. Changes in knowledge and competence were measured using pre- and post-test learner analysis. Intent to change practice and potential patient impact were also measured. Data collection is ongoing.
Results: As of June 6, 2024, a total of 266 learners participated, with the leading learner specialties being gastroenterologists (64%). A subset of learners (n=158) completed pre- and post-test assessments. Baseline knowledge was lowest regarding how to optimally utilize biologic therapy in pediatric and adult patients with EoE. Post-education, learners demonstrated a positive change in knowledge/competence related to: impact of delayed diagnosis of EoE (29%); recent therapeutic advances (43%); optimal use of biologic therapies (56%); and evidence-based, multidisciplinary strategies to improve patient care (42%). Of the learners, 96% intended to make changes to their practice based on the activity. Based on learners’ self-report of the number of patients seen per week, this program potentially impacted 796 patient interactions. Nearly half (46%) of learners also expressed interest in receiving further education related to tailoring the selection of first-line and step-up therapies.
Discussion: Our findings showed that i) hybrid CME was effective in improving knowledge and competence among clinicians related to the management of EoE based on recent therapeutic advances, and ii) an ongoing need/interest among clinicians to learn more about the evolving treatment paradigm.
Disclosures:
Tamima Ashraf indicated no relevant financial relationships.
Evan Dellon: Abbott – Consultant. AbbVie – Consultant. Adare/Ellodi – Consultant, Grant/Research Support. Aimmune – Consultant. Akesobio – Consultant. Alfasigma – Consultant. ALK – Consultant. Allakos – Consultant, Grant/Research Support. Amgen – Consultant. Aqilion – Consultant, Grant/Research Support. Arena/Pfizer – Consultant, Grant/Research Support. Aslan – Consultant. AstraZeneca – Consultant, Grant/Research Support. Avir – Consultant. Biorasi – Consultant. Calypso – Consultant. Celgene/Receptos/BMS – Consultant, Grant/Research Support. Celldex – Consultant. Dr. Falk Pharma – Consultant. Eli Lilly – Consultant. EsoCap – Consultant. Eupraxia – Consultant, Grant/Research Support. Ferring – Consultant, Grant/Research Support. GlaxoSmithKline – Consultant, Grant/Research Support. Gossamer Bio – Consultant. Holoclara – Consultant. Holoclara – Grant/Research Support. Invea – Consultant. Invea – Grant/Research Support. Knightpoint – Consultant. Landos – Consultant. LucidDx – Consultant. Meritage – Grant/Research Support. Miraca – Grant/Research Support. Morphic – Consultant. Nexstone Immunology/Uniquity – Consultant. Nutricia – Consultant, Grant/Research Support. Parexel/Calyx – Consultant. Phathom – Consultant. Regeneron Pharmaceuticals Inc. – Consultant, Grant/Research Support. Revolo – Consultant, Grant/Research Support. Robarts/Alimentiv – Consultant. Salix – Consultant. Sanofi – Consultant. Shire/Takeda – Consultant, Grant/Research Support. Target RWE – Consultant. Upstream Bio – Consultant.
Meghan Coulehan indicated no relevant financial relationships.
Emily Kitterman indicated no relevant financial relationships.
Aisha Suhail indicated no relevant financial relationships.
Tamima Ashraf, PhD1, Evan S.. Dellon, MD, MPH, FACG2, Meghan Coulehan, MPH1, Emily Kitterman, 1, Aisha Suhail, 1. P0483 - Bridging Knowledge and Competence Gaps Regarding Recent Therapeutic advances in Eosinophilic Esophagitis: Effectiveness of Continuing Medical Education, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
