Sunday Poster Session
Category: Esophagus
P0490 - Artificial Intelligence for Risk Prediction: A Simple, Explainable Machine Learning Model Predicts Incident Dysplasia or Malignancy in Barrett’s Esophagus
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- AR
Ashwin Rao, MD
Baylor College of Medicine
Houston, TX
Presenting Author(s)
Ashwin Rao, MD1, Jasmine Haydel, MD1, Samuel Ma, 1, Theresa Nguyen-Wenker, MD, PhD2, Hashem El-Serag, MD, MPH1
1Baylor College of Medicine, Houston, TX; 2Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX
Introduction: Level of dysplasia in Barrett’s Esophagus (BE) is associated with progression to esophageal adenocarcinoma (EAC). While non-dysplastic BE (NDBE) presents low annual risk (< 0.3%), persistent low-grade dysplasia (LGD) and high-grade dysplasia (HGD) have higher risk (13% and >20%, respectively) and ablation offers cure. Identifying patients likely to develop dysplasia or malignancy is critical for effective surveillance and treatment. We assess performance of machine learning (ML) models in predicting incident dysplasia or malignancy in a VA cohort
Methods: We analyzed data from 608 patients diagnosed with NDBE at the Michael E Debakey VA from Nov 1990-Jan 2019, with follow-up through Dec 2023. Progressors were defined as patients who developed persistent LGD, HGD, or EAC within five years of index EGD. The cohort was split into training (75%) and test (25%) sets. Six models were evaluated, including logistic regression and high complexity ML models. Steps included: variable selection (expert opinion, recursive feature elimination), data processing, addressing class imbalance (synthetic minority oversampling), hyperparameter tuning (grid search), and model comparison (cross validation, CV)
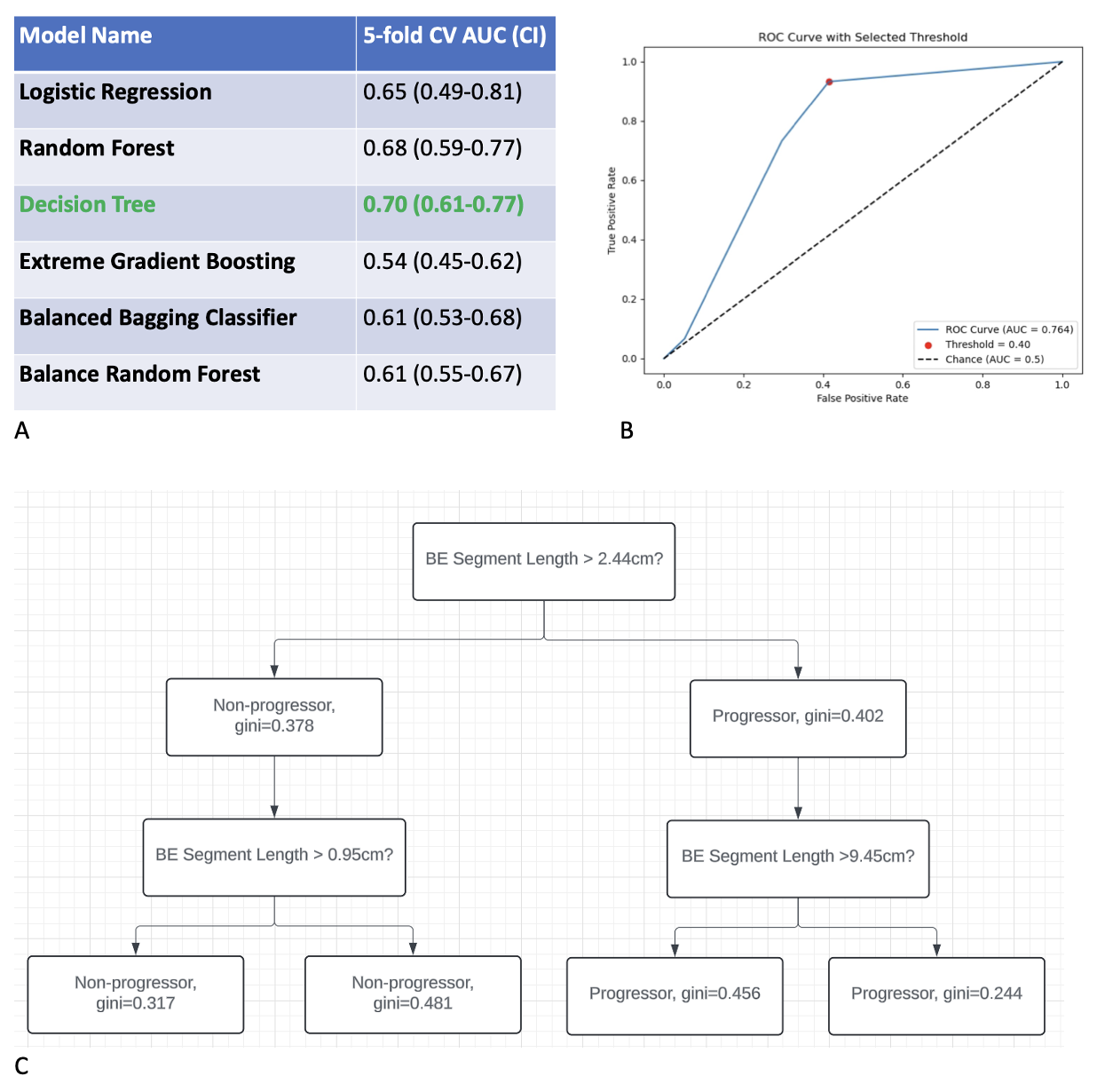
Results: Of 598 qualifying patients, 61 (10.2%) progressed. Longer BE segment and indefinite/nonpersistent LGD pathology were associated with higher risk of progression in unadjusted analyses (Table 1). Multivariate analysis confirmed BE segment as a predictor (OR 1.26; 95% CI 1.17-1.36 for each 1 cm increase). A decision tree (DT) model, using only BE segment length, achieved highest discrimination with CV AUROC=0.70 and test AUROC=0.76 (Figure 1A,B), excellent sensitivity (93.3%), and adequate calibration (brier score 0.18). It identified segment lengths for risk stratification: < 0.95cm (very low risk), 0.95-2.44cm (low risk), 2.44-9.45cm (moderate risk), >9.45cm (high risk) (Figure 1C)
Discussion: A simple, explainable DT model achieved excellent discrimination, sensitivity, and adequate calibration in predicting BE progressors, outperforming traditional regression and more complex ML models. Findings align with ESGE guidelines suggesting tailored surveillance based on segment length and provide actionable thresholds: < 1 cm (no surveillance), 1-2.5cm (lengthen surveillance to 5 years), 2.5-9.5cm (shorten to 3 years), and >9.5cm (consider intensive strategies, i.e. wide area tissue sampling). These results, pending validation in a national VA cohort, offer a practical ML-based tool for BE surveillance
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ashwin Rao, MD1, Jasmine Haydel, MD1, Samuel Ma, 1, Theresa Nguyen-Wenker, MD, PhD2, Hashem El-Serag, MD, MPH1. P0490 - Artificial Intelligence for Risk Prediction: A Simple, Explainable Machine Learning Model Predicts Incident Dysplasia or Malignancy in Barrett’s Esophagus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Baylor College of Medicine, Houston, TX; 2Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX
Introduction: Level of dysplasia in Barrett’s Esophagus (BE) is associated with progression to esophageal adenocarcinoma (EAC). While non-dysplastic BE (NDBE) presents low annual risk (< 0.3%), persistent low-grade dysplasia (LGD) and high-grade dysplasia (HGD) have higher risk (13% and >20%, respectively) and ablation offers cure. Identifying patients likely to develop dysplasia or malignancy is critical for effective surveillance and treatment. We assess performance of machine learning (ML) models in predicting incident dysplasia or malignancy in a VA cohort
Methods: We analyzed data from 608 patients diagnosed with NDBE at the Michael E Debakey VA from Nov 1990-Jan 2019, with follow-up through Dec 2023. Progressors were defined as patients who developed persistent LGD, HGD, or EAC within five years of index EGD. The cohort was split into training (75%) and test (25%) sets. Six models were evaluated, including logistic regression and high complexity ML models. Steps included: variable selection (expert opinion, recursive feature elimination), data processing, addressing class imbalance (synthetic minority oversampling), hyperparameter tuning (grid search), and model comparison (cross validation, CV)
Results: Of 598 qualifying patients, 61 (10.2%) progressed. Longer BE segment and indefinite/nonpersistent LGD pathology were associated with higher risk of progression in unadjusted analyses (Table 1). Multivariate analysis confirmed BE segment as a predictor (OR 1.26; 95% CI 1.17-1.36 for each 1 cm increase). A decision tree (DT) model, using only BE segment length, achieved highest discrimination with CV AUROC=0.70 and test AUROC=0.76 (Figure 1A,B), excellent sensitivity (93.3%), and adequate calibration (brier score 0.18). It identified segment lengths for risk stratification: < 0.95cm (very low risk), 0.95-2.44cm (low risk), 2.44-9.45cm (moderate risk), >9.45cm (high risk) (Figure 1C)
Discussion: A simple, explainable DT model achieved excellent discrimination, sensitivity, and adequate calibration in predicting BE progressors, outperforming traditional regression and more complex ML models. Findings align with ESGE guidelines suggesting tailored surveillance based on segment length and provide actionable thresholds: < 1 cm (no surveillance), 1-2.5cm (lengthen surveillance to 5 years), 2.5-9.5cm (shorten to 3 years), and >9.5cm (consider intensive strategies, i.e. wide area tissue sampling). These results, pending validation in a national VA cohort, offer a practical ML-based tool for BE surveillance
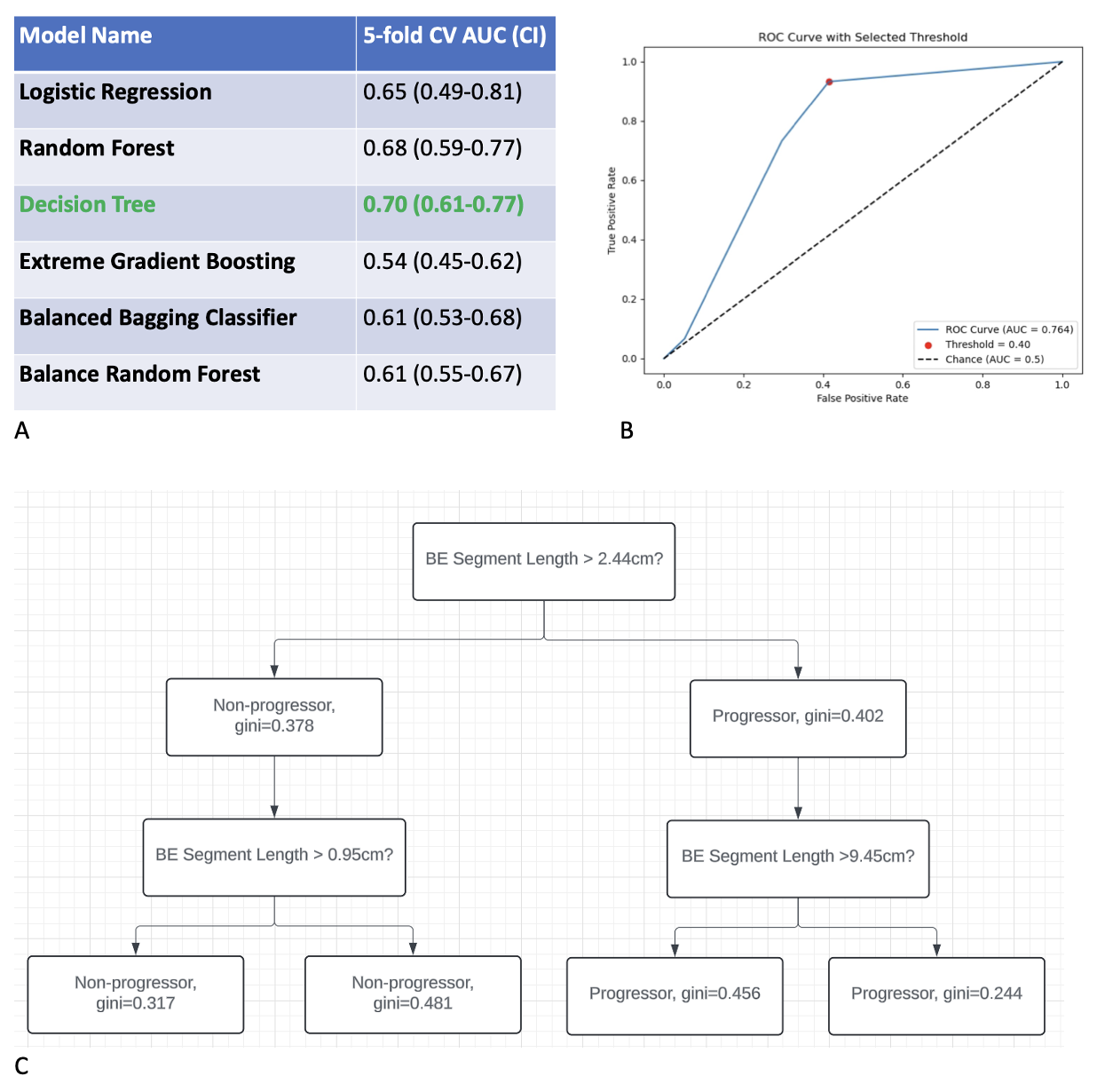
Figure: Figure 1. Decision Tree (DT) cross validation, test performance, explainability analysis. Comparison of traditional logistic regression and machine learning models during cross validation showed a DT-based model achieved the highest discrimination (Figure 1A). DT-based model performance on the test set maintained excellent discrimination, with an AUROC of 0.76 (Figure 1B). Explainability analysis of the DT-based model showed important segment length thresholds for predicting progression; lower Gini impurity scores indicate higher confidence in predictions, reflecting risk of progression.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ashwin Rao indicated no relevant financial relationships.
Jasmine Haydel indicated no relevant financial relationships.
Samuel Ma indicated no relevant financial relationships.
Theresa Nguyen-Wenker indicated no relevant financial relationships.
Hashem El-Serag indicated no relevant financial relationships.
Ashwin Rao, MD1, Jasmine Haydel, MD1, Samuel Ma, 1, Theresa Nguyen-Wenker, MD, PhD2, Hashem El-Serag, MD, MPH1. P0490 - Artificial Intelligence for Risk Prediction: A Simple, Explainable Machine Learning Model Predicts Incident Dysplasia or Malignancy in Barrett’s Esophagus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
