Sunday Poster Session
Category: Esophagus
P0491 - Food for Thought: The Need for Imaging in Esophageal Food Bolus
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- RM
Raakhi Menon, DO
University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Raakhi Menon, DO, Muhammad Mushtaq, DO, Kian Abdul-Baki, DO, Eric Margulies, MD, Brooke Corning, MD
University of Texas Medical Branch, Galveston, TX
Introduction: Esophageal food bolus impaction is a medical emergency. While most foreign objects and food boluses pass spontaneously, 10% to 20% may require endoscopic removal. Delaying esophagogastroduodenoscopy (EGD) is discouraged, as prompt removal within 24 hours is recommended by the American Society for Gastrointestinal Endoscopy (ASGE). Current gastrointestinal treatment guidelines advise against obtaining radiographs before endoscopic evaluation in suspected uncomplicated, nonbony esophageal food bolus cases.
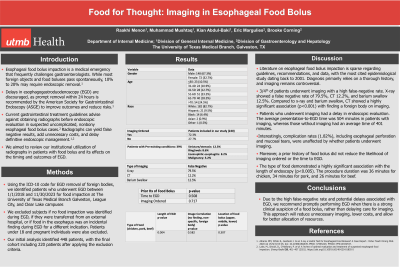
Methods: We searched our institution's electronic medical record system using the relevant ICD-10 code for EGD removal of foreign bodies. Our retrospective study included procedures performed at our institution between 1/1/2018 and 11/30/2023, focusing on patients who underwent EGD for esophageal food impaction. We excluded subjects if EGD was not necessary for food bolus removal, no food impaction was identified, they were transferred from an external hospital, or food in the esophagus was an incidental finding during EGD for another indication. Out of 448 EGD procedures coded, we included 220 in our analysis.
Results: Our data showed that males (67.5%), individuals over 70 years old (24.5%), and Caucasians (82.7%) had the highest rates of food boluses. Among individuals with food boluses, 72.2% had imaging ordered in the ED, and 39% had pre-existing conditions.
Compared to X-ray and barium swallow, CT showed a highly significant association (p< 0.001) with finding a foreign body on imaging. X-ray showed a false negative rate of 79.5%, CT 12.2%, and barium swallow 12.5%. Patients who underwent imaging had an average presentation-to-EGD time of 504 minutes, whereas those without imaging had an average time of 401 minutes. The overall complication rate stood at 1.82%, evenly distributed between the imaging and non-imaging cohorts at 50% each.
Discussion: Literature on esophageal food bolus impaction is sparse regarding guidelines, recommendations, and data, with the most cited epidemiological study dating back to 2001. Diagnosis primarily relies on a thorough history, and the use of imaging remains controversial. In our patient cohort, 60% underwent X-rays, with a notable false negative rate of 79.5%. Complication rates, including esophageal perforation and mucosal tears, were unaffected by whether patients underwent imaging or not. Our recommendation is to proceed with EGD promptly when clinical suspicion for food bolus is high, rather than delaying for imaging.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Raakhi Menon, DO, Muhammad Mushtaq, DO, Kian Abdul-Baki, DO, Eric Margulies, MD, Brooke Corning, MD. P0491 - Food for Thought: The Need for Imaging in Esophageal Food Bolus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Texas Medical Branch, Galveston, TX
Introduction: Esophageal food bolus impaction is a medical emergency. While most foreign objects and food boluses pass spontaneously, 10% to 20% may require endoscopic removal. Delaying esophagogastroduodenoscopy (EGD) is discouraged, as prompt removal within 24 hours is recommended by the American Society for Gastrointestinal Endoscopy (ASGE). Current gastrointestinal treatment guidelines advise against obtaining radiographs before endoscopic evaluation in suspected uncomplicated, nonbony esophageal food bolus cases.
Methods: We searched our institution's electronic medical record system using the relevant ICD-10 code for EGD removal of foreign bodies. Our retrospective study included procedures performed at our institution between 1/1/2018 and 11/30/2023, focusing on patients who underwent EGD for esophageal food impaction. We excluded subjects if EGD was not necessary for food bolus removal, no food impaction was identified, they were transferred from an external hospital, or food in the esophagus was an incidental finding during EGD for another indication. Out of 448 EGD procedures coded, we included 220 in our analysis.
Results: Our data showed that males (67.5%), individuals over 70 years old (24.5%), and Caucasians (82.7%) had the highest rates of food boluses. Among individuals with food boluses, 72.2% had imaging ordered in the ED, and 39% had pre-existing conditions.
Compared to X-ray and barium swallow, CT showed a highly significant association (p< 0.001) with finding a foreign body on imaging. X-ray showed a false negative rate of 79.5%, CT 12.2%, and barium swallow 12.5%. Patients who underwent imaging had an average presentation-to-EGD time of 504 minutes, whereas those without imaging had an average time of 401 minutes. The overall complication rate stood at 1.82%, evenly distributed between the imaging and non-imaging cohorts at 50% each.
Discussion: Literature on esophageal food bolus impaction is sparse regarding guidelines, recommendations, and data, with the most cited epidemiological study dating back to 2001. Diagnosis primarily relies on a thorough history, and the use of imaging remains controversial. In our patient cohort, 60% underwent X-rays, with a notable false negative rate of 79.5%. Complication rates, including esophageal perforation and mucosal tears, were unaffected by whether patients underwent imaging or not. Our recommendation is to proceed with EGD promptly when clinical suspicion for food bolus is high, rather than delaying for imaging.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Raakhi Menon indicated no relevant financial relationships.
Muhammad Mushtaq indicated no relevant financial relationships.
Kian Abdul-Baki indicated no relevant financial relationships.
Eric Margulies indicated no relevant financial relationships.
Brooke Corning indicated no relevant financial relationships.
Raakhi Menon, DO, Muhammad Mushtaq, DO, Kian Abdul-Baki, DO, Eric Margulies, MD, Brooke Corning, MD. P0491 - Food for Thought: The Need for Imaging in Esophageal Food Bolus, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
