Sunday Poster Session
Category: Esophagus
P0495 - Comparative Outcomes of Gastroesophageal Reflux Disease, Nonerosive Reflux Disease, and Erosive Esophagitis in Patients Undergoing Roux-en-Y Gastric Bypass versus Sleeve Gastrectomy for Weight Loss
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Rishi Chowdhary, MD
Metrohealth Medical Center
Cleveland, OH
Presenting Author(s)
Rishi Chowdhary, MD1, Benjamin Liu, MD2, Ronnie Fass, MD3
1Metrohealth Medical Center, Cleveland, OH; 2MetroHealth Medical Center, Cleveland, OH; 3Case Western Reserve University / MetroHealth, Cleveland, OH
Introduction: Laparoscopic Sleeve Gastrectomy (LSG) and Roux-En-Y Gastric Bypass (RYGB) are the most common bariatric surgeries. Recent studies raised concerns about de novo GERD, erosive esophagitis, and Barrett's esophagus (BE) following LSG. We examined this association using the TriNetX database.
Methods: We used TriNetX, a global electronic health record database, to study adult patients with BMI ≥35 kg/m² undergoing bariatric surgery. Patients were divided into two cohorts based on whether they underwent LSG or RYGB. Exclusion criteria included history of upper gastrointestinal malignancies, scleroderma, GERD prior to surgery, or major upper abdominal or thoracic surgery. Cohorts underwent 1:1 propensity score matching based on age, demographics, initial BMI, type 2 diabetes with complications, and opioid usage. We compared outcomes 10 years post-surgery using Kaplan-Meier and Cox proportional hazards models. Outcomes included new GERD, non-erosive reflux disease (NERD), erosive reflux disease (ERD), and Barrett's esophagus with (BWD) or without dysplasia (BWOD). Sub-analyses were based on initial BMI categories ( >50 and 35-50).
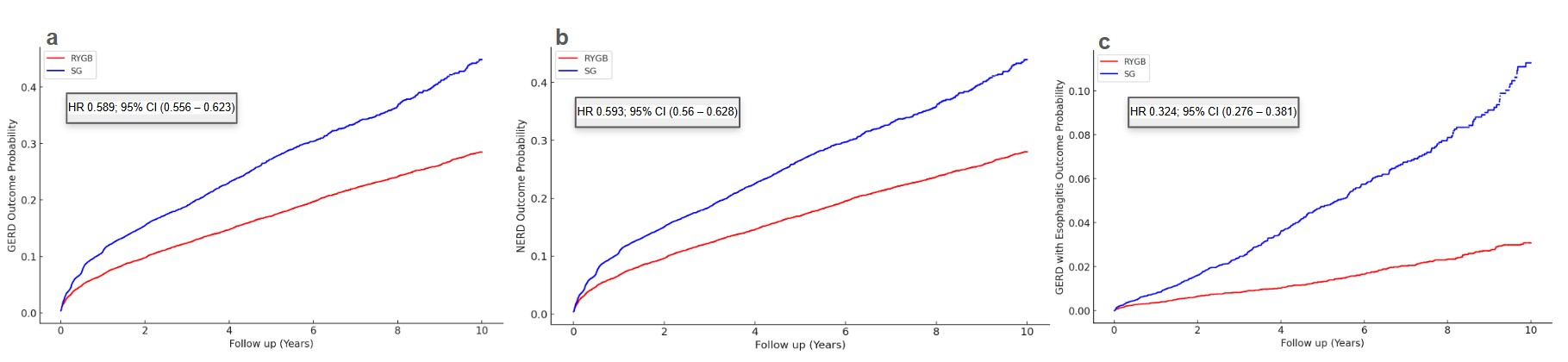
Results: The unmatched RYGB cohort included 16,137 patients, and the LSG cohort had 31,358 patients. After propensity matching, each cohort had 15,245 patients. The mean follow-up was 1,843 days for RYGB and 1,216 days for LSG. Both cohorts lost weight rapidly: RYGB patients went from a BMI of 47 ± 7.32 to 32.38 ± 6.73 in 1-2 years, and LSG patients from 46.7 ± 7.6 to 35.17 ± 7.41. RYGB patients had a GERD event rate of 29.38 per 1,000 person-years; LSG had 54.51 per 1,000 person-years. Cox-proportional hazards models showed RYGB patients had a 41.1% lower risk of GERD than LSG (HR 0.589; 95% CI 0.556–0.623). RYGB patients had a 40.7% lower risk of NERD (HR 0.593; 95% CI 0.56–0.628). For ERD, RYGB had 3.01 events per 1,000 person-years, LSG had 8.96; RYGB had a 67.6% reduced risk (HR 0.324; 95% CI 0.276–0.381). There were no significant differences in BWD (HR 0.863; 95% CI 0.294–2.536) or BWOD (HR 1.047; 95% CI 0.703–1.559), though BWD analysis was limited by 10 events in each cohort. Sub-analyses by initial BMI 35-50 and >50 showed consistent trends.
Discussion: Despite significant weight loss in both cohorts, this study highlights differences in GERD outcomes between RYGB and LSG over 10 years. RYGB's anatomical modifications may offer protection against GERD compared to LSG. Further prospective studies are needed to validate these results and guide clinical decisions.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rishi Chowdhary, MD1, Benjamin Liu, MD2, Ronnie Fass, MD3. P0495 - Comparative Outcomes of Gastroesophageal Reflux Disease, Nonerosive Reflux Disease, and Erosive Esophagitis in Patients Undergoing Roux-en-Y Gastric Bypass versus Sleeve Gastrectomy for Weight Loss, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Metrohealth Medical Center, Cleveland, OH; 2MetroHealth Medical Center, Cleveland, OH; 3Case Western Reserve University / MetroHealth, Cleveland, OH
Introduction: Laparoscopic Sleeve Gastrectomy (LSG) and Roux-En-Y Gastric Bypass (RYGB) are the most common bariatric surgeries. Recent studies raised concerns about de novo GERD, erosive esophagitis, and Barrett's esophagus (BE) following LSG. We examined this association using the TriNetX database.
Methods: We used TriNetX, a global electronic health record database, to study adult patients with BMI ≥35 kg/m² undergoing bariatric surgery. Patients were divided into two cohorts based on whether they underwent LSG or RYGB. Exclusion criteria included history of upper gastrointestinal malignancies, scleroderma, GERD prior to surgery, or major upper abdominal or thoracic surgery. Cohorts underwent 1:1 propensity score matching based on age, demographics, initial BMI, type 2 diabetes with complications, and opioid usage. We compared outcomes 10 years post-surgery using Kaplan-Meier and Cox proportional hazards models. Outcomes included new GERD, non-erosive reflux disease (NERD), erosive reflux disease (ERD), and Barrett's esophagus with (BWD) or without dysplasia (BWOD). Sub-analyses were based on initial BMI categories ( >50 and 35-50).
Results: The unmatched RYGB cohort included 16,137 patients, and the LSG cohort had 31,358 patients. After propensity matching, each cohort had 15,245 patients. The mean follow-up was 1,843 days for RYGB and 1,216 days for LSG. Both cohorts lost weight rapidly: RYGB patients went from a BMI of 47 ± 7.32 to 32.38 ± 6.73 in 1-2 years, and LSG patients from 46.7 ± 7.6 to 35.17 ± 7.41. RYGB patients had a GERD event rate of 29.38 per 1,000 person-years; LSG had 54.51 per 1,000 person-years. Cox-proportional hazards models showed RYGB patients had a 41.1% lower risk of GERD than LSG (HR 0.589; 95% CI 0.556–0.623). RYGB patients had a 40.7% lower risk of NERD (HR 0.593; 95% CI 0.56–0.628). For ERD, RYGB had 3.01 events per 1,000 person-years, LSG had 8.96; RYGB had a 67.6% reduced risk (HR 0.324; 95% CI 0.276–0.381). There were no significant differences in BWD (HR 0.863; 95% CI 0.294–2.536) or BWOD (HR 1.047; 95% CI 0.703–1.559), though BWD analysis was limited by 10 events in each cohort. Sub-analyses by initial BMI 35-50 and >50 showed consistent trends.
Discussion: Despite significant weight loss in both cohorts, this study highlights differences in GERD outcomes between RYGB and LSG over 10 years. RYGB's anatomical modifications may offer protection against GERD compared to LSG. Further prospective studies are needed to validate these results and guide clinical decisions.
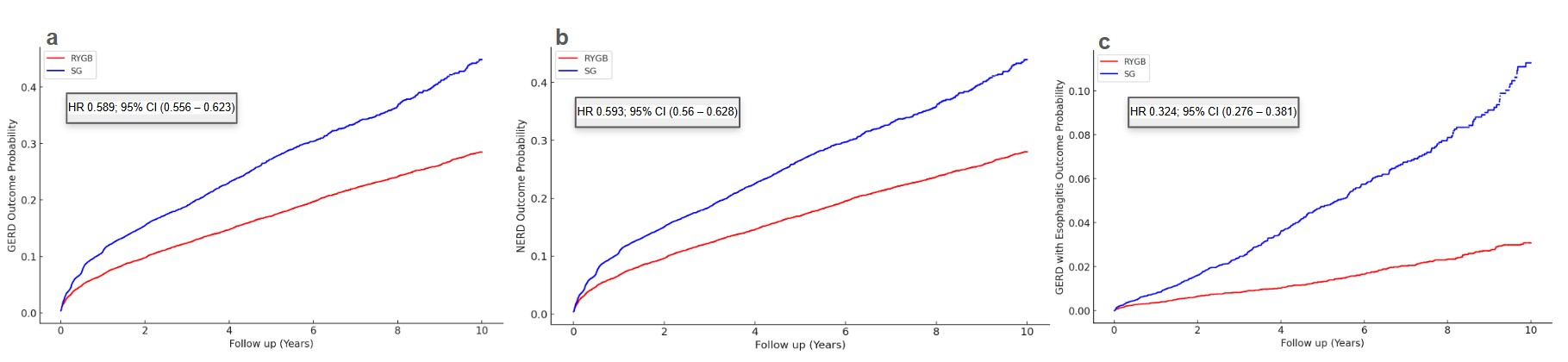
Figure: Figure 1. Kaplan-Meier graph showing a) GERD, b) Non-erosive reflux disease, and c) Erosive esophagitis outcomes over the years.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rishi Chowdhary indicated no relevant financial relationships.
Benjamin Liu indicated no relevant financial relationships.
Ronnie Fass indicated no relevant financial relationships.
Rishi Chowdhary, MD1, Benjamin Liu, MD2, Ronnie Fass, MD3. P0495 - Comparative Outcomes of Gastroesophageal Reflux Disease, Nonerosive Reflux Disease, and Erosive Esophagitis in Patients Undergoing Roux-en-Y Gastric Bypass versus Sleeve Gastrectomy for Weight Loss, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
