Sunday Poster Session
Category: Esophagus
P0511 - Correlation of Esophageal Motility Abnormality on Video Fluoroscopic Study With Findings on High Resolution Esophageal Manometry
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Eleanor Belilos, MD
Rush University Medical Center
Chicago, IL
Presenting Author(s)
Eleanor Belilos, MD, Gabrielle Klugman, , Yanyu Zhang, MS, Rana Abraham, MD
Rush University Medical Center, Chicago, IL
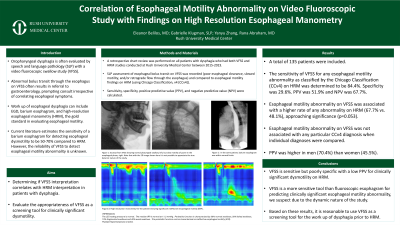
Introduction: Oropharyngeal dysphagia is often evaluated by speech and language pathology (SLP) with a video fluoroscopic swallow study (VFSS). Abnormal bolus transit through the esophagus often results in referral to gastroenterology, prompting consult irrespective of correlating esophageal symptoms. Work up can include EGD and high-resolution esophageal manometry (HRM), the gold standard in evaluating esophageal motility. Current literature estimates the sensitivity of a fluoroscopic esophagram for detecting esophageal dysmotility to be 50-70% compared to HRM. However, the reliability of VFSS to screen for esophageal motility abnormality is unknown. The aim of this study was to evaluate the appropriateness of VFSS as a screening tool for clinically significant dysmotility by determining if VFSS interpretation correlates with HRM interpretation in patients with dysphagia.
Methods: A retrospective chart review was performed on all patients with dysphagia who had both VFSS and HRM studies conducted at a single institution between 2015-2023. SLP assessment of esophageal bolus transit on VFSS was recorded (poor esophageal clearance, slowed motility, and/or retrograde flow through the esophagus) and compared to esophageal motility findings on HRM (using Chicago Classification, v4 [CCv4]). Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated.
Results: A total of 135 patients were included. The sensitivity of VFSS for any abnormal esophageal motility abnormality as classified by the Chicago Classification (CCv4) on HRM was determined to be 84.4%. Specificity was 29.6%. PPV was 51.9% and NPV was 67.7%. Esophageal motility abnormality on VFSS was associated with a higher rate of any abnormality on HRM (67.7% vs. 48.1%), approaching significance (p=0.053), however was not associated with any particular CCv4 diagnosis when individual diagnoses were compared. PPV was higher in men (70.4%) than women (45.5%).
Discussion: VFSS is sensitive but poorly specific with a low PPV for clinically significant dysmotility on HRM. Furthermore, VFSS is a more sensitive tool than fluoroscopic esophagram for predicting clinically significant esophageal motility abnormality, we suspect due to the dynamic nature of the study. Based on these results, it is reasonable to use VFSS as a screening tool for further work up of dysphagia with HRM, an invasive procedure that often comes without benefit to the patient.
Disclosures:
Eleanor Belilos, MD, Gabrielle Klugman, , Yanyu Zhang, MS, Rana Abraham, MD. P0511 - Correlation of Esophageal Motility Abnormality on Video Fluoroscopic Study With Findings on High Resolution Esophageal Manometry, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Rush University Medical Center, Chicago, IL
Introduction: Oropharyngeal dysphagia is often evaluated by speech and language pathology (SLP) with a video fluoroscopic swallow study (VFSS). Abnormal bolus transit through the esophagus often results in referral to gastroenterology, prompting consult irrespective of correlating esophageal symptoms. Work up can include EGD and high-resolution esophageal manometry (HRM), the gold standard in evaluating esophageal motility. Current literature estimates the sensitivity of a fluoroscopic esophagram for detecting esophageal dysmotility to be 50-70% compared to HRM. However, the reliability of VFSS to screen for esophageal motility abnormality is unknown. The aim of this study was to evaluate the appropriateness of VFSS as a screening tool for clinically significant dysmotility by determining if VFSS interpretation correlates with HRM interpretation in patients with dysphagia.
Methods: A retrospective chart review was performed on all patients with dysphagia who had both VFSS and HRM studies conducted at a single institution between 2015-2023. SLP assessment of esophageal bolus transit on VFSS was recorded (poor esophageal clearance, slowed motility, and/or retrograde flow through the esophagus) and compared to esophageal motility findings on HRM (using Chicago Classification, v4 [CCv4]). Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated.
Results: A total of 135 patients were included. The sensitivity of VFSS for any abnormal esophageal motility abnormality as classified by the Chicago Classification (CCv4) on HRM was determined to be 84.4%. Specificity was 29.6%. PPV was 51.9% and NPV was 67.7%. Esophageal motility abnormality on VFSS was associated with a higher rate of any abnormality on HRM (67.7% vs. 48.1%), approaching significance (p=0.053), however was not associated with any particular CCv4 diagnosis when individual diagnoses were compared. PPV was higher in men (70.4%) than women (45.5%).
Discussion: VFSS is sensitive but poorly specific with a low PPV for clinically significant dysmotility on HRM. Furthermore, VFSS is a more sensitive tool than fluoroscopic esophagram for predicting clinically significant esophageal motility abnormality, we suspect due to the dynamic nature of the study. Based on these results, it is reasonable to use VFSS as a screening tool for further work up of dysphagia with HRM, an invasive procedure that often comes without benefit to the patient.
Disclosures:
Eleanor Belilos indicated no relevant financial relationships.
Gabrielle Klugman indicated no relevant financial relationships.
Yanyu Zhang indicated no relevant financial relationships.
Rana Abraham indicated no relevant financial relationships.
Eleanor Belilos, MD, Gabrielle Klugman, , Yanyu Zhang, MS, Rana Abraham, MD. P0511 - Correlation of Esophageal Motility Abnormality on Video Fluoroscopic Study With Findings on High Resolution Esophageal Manometry, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
