Sunday Poster Session
Category: Esophagus
P0540 - Bridge Over Swallowed Waters: A Case of Esophageal Mucosal Bridge-Induced Dysphagia
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

David Okuampa, MD
Louisiana State University Health
Shreveport, LA
Presenting Author(s)
David Okuampa, MD1, Gabrielle Sanford, MD1, Aditya Vyas, MD1, Farhan Mohiuddin, MD1, Sudha Pandit, MD2
1Louisiana State University Health, Shreveport, LA; 2LSU Health, Shreveport, LA
Introduction: An esophageal mucosal bridge (EMB) is a cord-like connection across the esophageal lumen, often discovered incidentally during esophagogastroduodenoscopy (EGD). EMB can be congenital or acquired due to factors like reflux esophagitis, radiation therapy, Crohn’s disease, and infections (HIV/AIDS, candidiasis). We present a case of EMB in a patient with multiple risk factors, successfully treated with endoscopic electrosurgical intervention, resulting in complete symptom resolution.
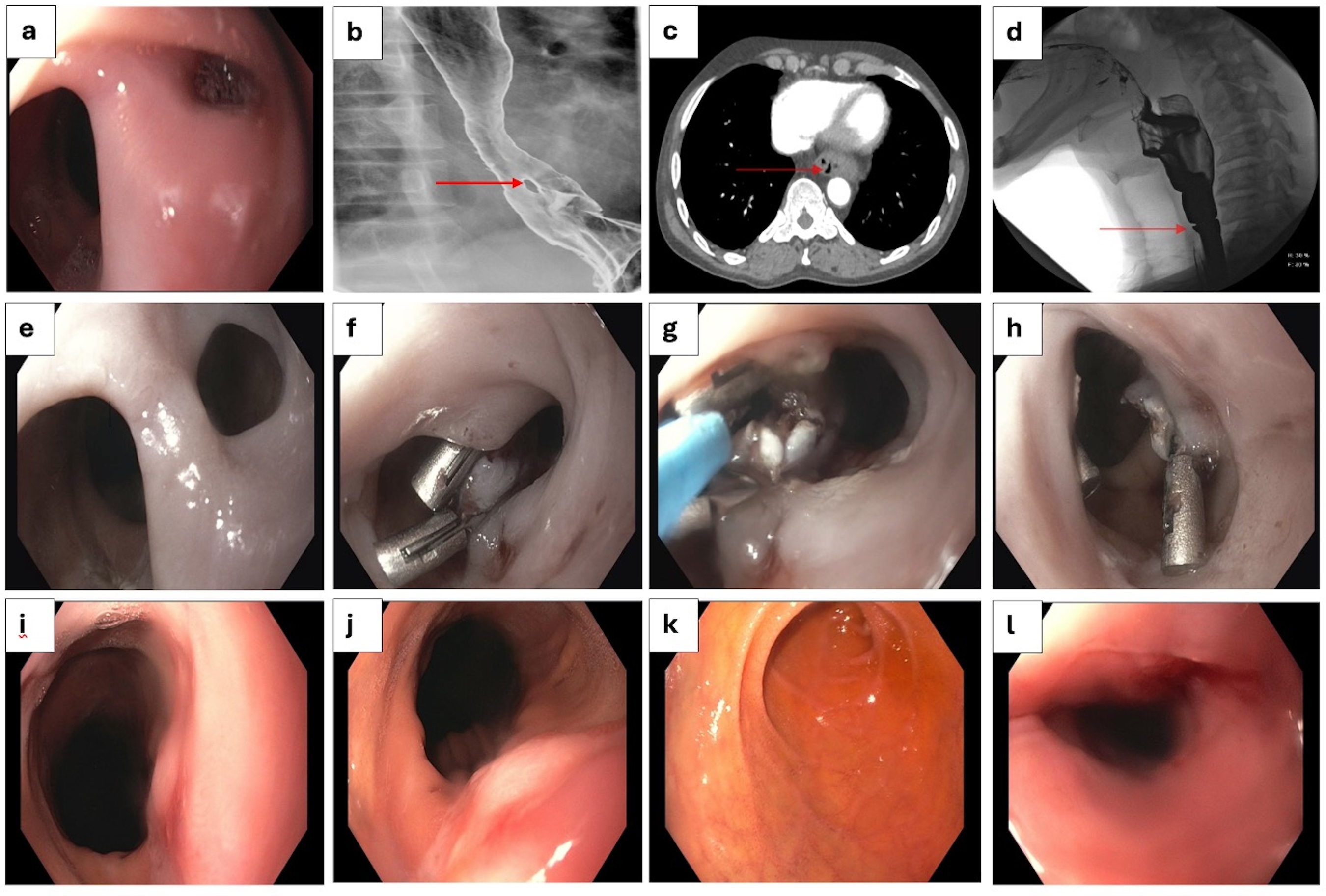
Case Description/Methods: A 67-year-old man with a medical history of HIV, radiation-induced esophagitis requiring multiple EGDs with dilation, GERD, and metastatic prostate cancer post-chemoradiation. He presented to the GI clinic with progressive dysphagia for solid foods and weight loss. His last EGD 2 years ago was concerning for a fistula versus diverticulum in the distal esophagus. An upper GI series showed strictures and filling defect in the distal esophagus, correlating with CT imaging (Fig 1a-d).
A recent EGD showed a 10 mm deep mucosal bridge in the distal esophagus, 38 cm from the incisors, creating a dual lumen appearance. Hemo-clips were placed at the ends of the mucosal bridge. An attempt to transect the mucosal bridge with an endoscopic needle knife was unsuccessful, so a 15 mm hot polypectomy snare tip with the coagulation current only was used to disrupt the bridge successfully. Biopsy showed no abnormalities. Follow-up at 4 weeks revealed significant improvement, with resolution of the bridge and mild fibrosis remaining (Fig 1e-l).
Discussion: Our patient, with risk factors including HIV, GERD, and radiation esophagitis, represents the first reported case of EMB with three contributing factors. The initial fistula observed likely indicated the formation of the mucosal bridge, but since the patient was asymptomatic then, no intervention was undertaken.
Endoscopic ablation such as Argon plasma coagulation and electrosurgical intervention remains the first-line therapy for EMB. Electrosurgical intervention, which involves placing hemo-clips at both ends of the bridge and ablating the tissue using a hot snare, hot biopsy forceps, or a needle knife, has proven to be safe and effective. In our patient's case, a hot polypectomy snare tip was used without any complications.
This case underscores the importance of considering EMB in patients with dysphagia and multiple risk factors. Endoscopic ablation techniques are effective, but further research is needed to determine the most optimal treatment methods.
Disclosures:
David Okuampa, MD1, Gabrielle Sanford, MD1, Aditya Vyas, MD1, Farhan Mohiuddin, MD1, Sudha Pandit, MD2. P0540 - Bridge Over Swallowed Waters: A Case of Esophageal Mucosal Bridge-Induced Dysphagia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Louisiana State University Health, Shreveport, LA; 2LSU Health, Shreveport, LA
Introduction: An esophageal mucosal bridge (EMB) is a cord-like connection across the esophageal lumen, often discovered incidentally during esophagogastroduodenoscopy (EGD). EMB can be congenital or acquired due to factors like reflux esophagitis, radiation therapy, Crohn’s disease, and infections (HIV/AIDS, candidiasis). We present a case of EMB in a patient with multiple risk factors, successfully treated with endoscopic electrosurgical intervention, resulting in complete symptom resolution.
Case Description/Methods: A 67-year-old man with a medical history of HIV, radiation-induced esophagitis requiring multiple EGDs with dilation, GERD, and metastatic prostate cancer post-chemoradiation. He presented to the GI clinic with progressive dysphagia for solid foods and weight loss. His last EGD 2 years ago was concerning for a fistula versus diverticulum in the distal esophagus. An upper GI series showed strictures and filling defect in the distal esophagus, correlating with CT imaging (Fig 1a-d).
A recent EGD showed a 10 mm deep mucosal bridge in the distal esophagus, 38 cm from the incisors, creating a dual lumen appearance. Hemo-clips were placed at the ends of the mucosal bridge. An attempt to transect the mucosal bridge with an endoscopic needle knife was unsuccessful, so a 15 mm hot polypectomy snare tip with the coagulation current only was used to disrupt the bridge successfully. Biopsy showed no abnormalities. Follow-up at 4 weeks revealed significant improvement, with resolution of the bridge and mild fibrosis remaining (Fig 1e-l).
Discussion: Our patient, with risk factors including HIV, GERD, and radiation esophagitis, represents the first reported case of EMB with three contributing factors. The initial fistula observed likely indicated the formation of the mucosal bridge, but since the patient was asymptomatic then, no intervention was undertaken.
Endoscopic ablation such as Argon plasma coagulation and electrosurgical intervention remains the first-line therapy for EMB. Electrosurgical intervention, which involves placing hemo-clips at both ends of the bridge and ablating the tissue using a hot snare, hot biopsy forceps, or a needle knife, has proven to be safe and effective. In our patient's case, a hot polypectomy snare tip was used without any complications.
This case underscores the importance of considering EMB in patients with dysphagia and multiple risk factors. Endoscopic ablation techniques are effective, but further research is needed to determine the most optimal treatment methods.
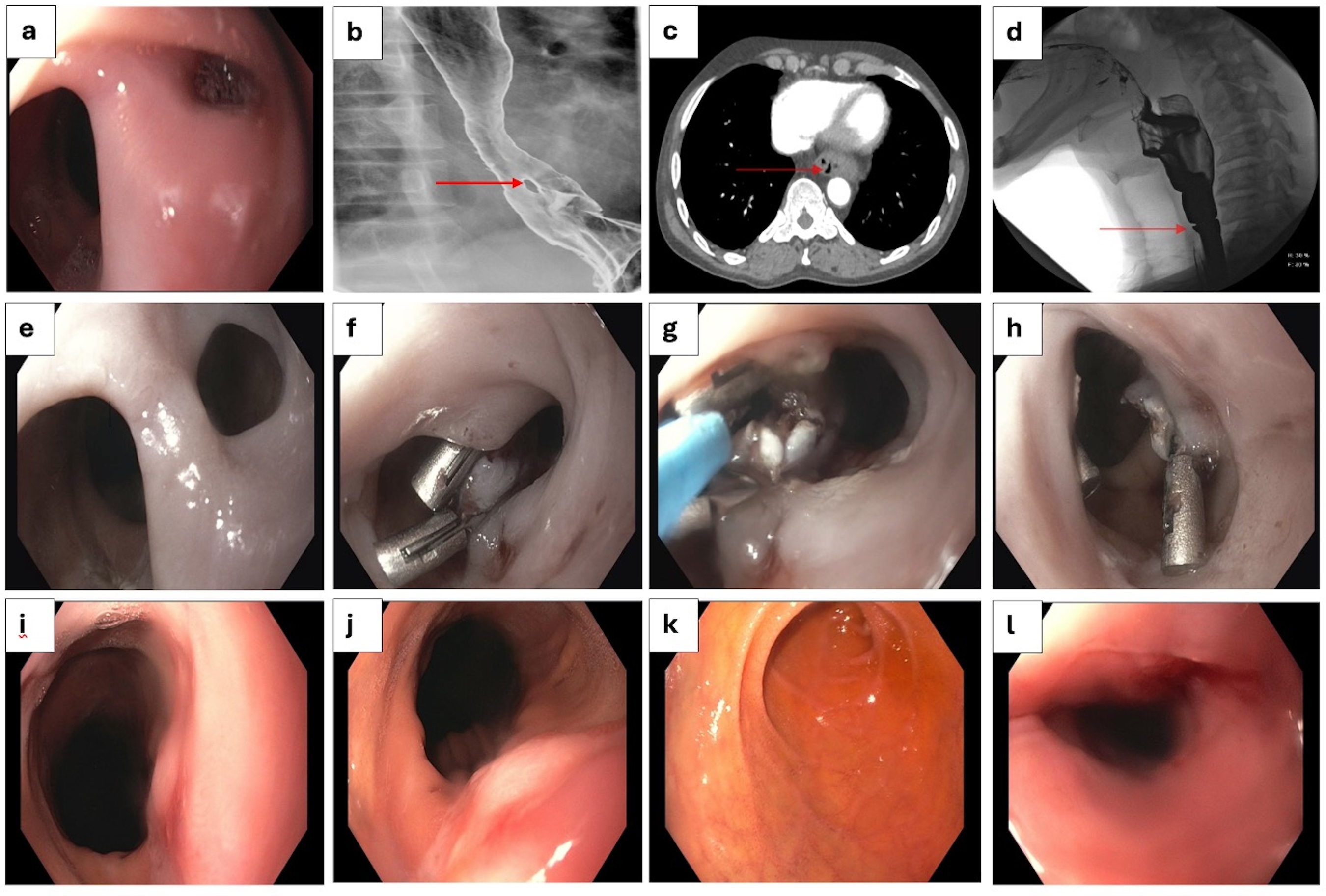
Figure: Figure 1a: Initial endoscopic finding concerning for a fistula vs diverticula in distal esophagus
Figure 1b-d: Upper GI series showing filling defect in distal esophagus, double lumen on CT, and circumferential strictures in cervical region
Figure 1e-f: Mucosal bridge at 38 cm from incisor and application of hemoclips .
Figure 1g-h: Disruption of the mucosal bridge with 15 mm flexible polypectomy snare tip.
Figure 1i-j: Normal appearing esophageal mucosa after 4 weeks
Figure 1k-l: Esophageal web and mucosal tear post dilation
Figure 1b-d: Upper GI series showing filling defect in distal esophagus, double lumen on CT, and circumferential strictures in cervical region
Figure 1e-f: Mucosal bridge at 38 cm from incisor and application of hemoclips .
Figure 1g-h: Disruption of the mucosal bridge with 15 mm flexible polypectomy snare tip.
Figure 1i-j: Normal appearing esophageal mucosa after 4 weeks
Figure 1k-l: Esophageal web and mucosal tear post dilation
Disclosures:
David Okuampa indicated no relevant financial relationships.
Gabrielle Sanford indicated no relevant financial relationships.
Aditya Vyas indicated no relevant financial relationships.
Farhan Mohiuddin indicated no relevant financial relationships.
Sudha Pandit indicated no relevant financial relationships.
David Okuampa, MD1, Gabrielle Sanford, MD1, Aditya Vyas, MD1, Farhan Mohiuddin, MD1, Sudha Pandit, MD2. P0540 - Bridge Over Swallowed Waters: A Case of Esophageal Mucosal Bridge-Induced Dysphagia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
