Sunday Poster Session
Category: Esophagus
P0542 - Pulmonary Hypertension and Downhill Varices: An Incidental Finding
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Bianca Thakkar, DO
University of Connecticut Health Center
Farmington, CT
Presenting Author(s)
Bianca Thakkar, DO1, Teresa Da Cunha, MD1, Rachael Hagen, DO2, Roopjeet K. Bath, MBBS3
1University of Connecticut Health Center, Farmington, CT; 2University of Connecticut Health, Farmington, CT; 3UConn Health, Farmington, CT
Introduction: Esophageal varices are dilated submucosal esophageal veins connecting the portal and systemic circulation. Compared to distal esophageal varices, downhill varices (DV) are a rare entity and can occur in the middle and proximal esophagus. DV usually results from an obstruction of the superior vena cava (SVC). Incidental DVs are rare and require further workup. We describe a case of a patient who presented with shortness of breath and melena and was found to have DVs.
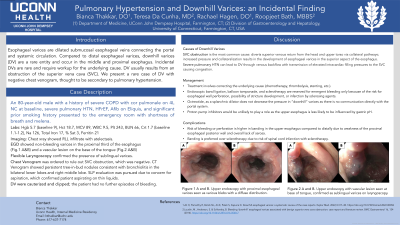
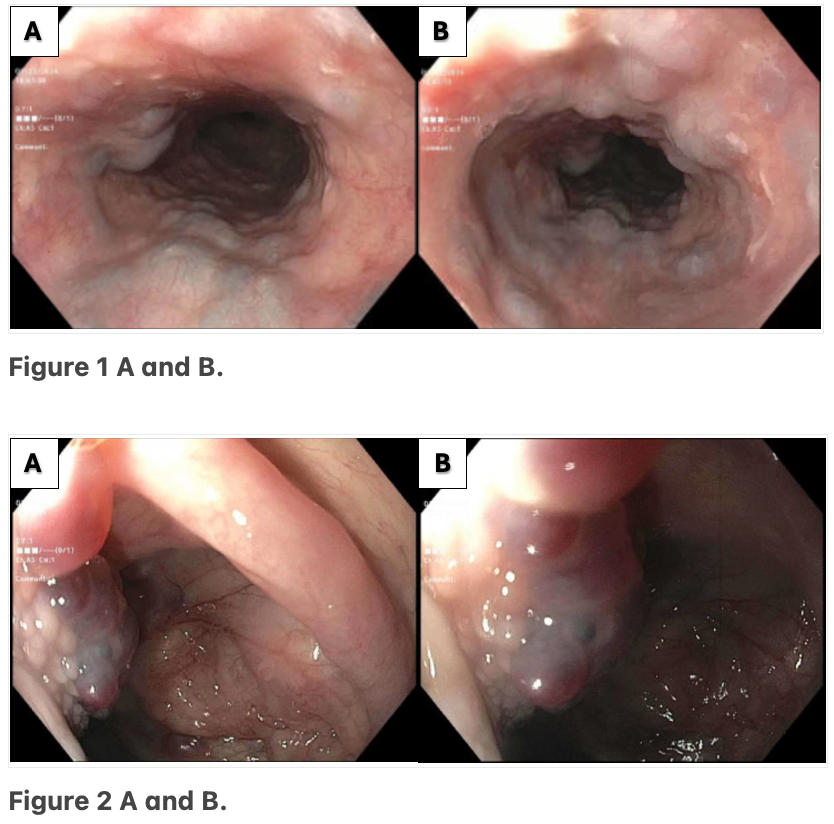
Case Description/Methods: An 80-year-old male with a history of chronic obstructive pulmonary disease, severe pulmonary hypertension, heart failure with reduced ejection fraction, and significant prior smoking history presented to the emergency room with shortness of breath and melena. He had a hemoglobin of 5.9 from a baseline of 9. After adequate resuscitation, an EGD was performed, which showed non-bleeding varices in the proximal third of the esophagus (Fig.1 A&B) and a vascular lesion on the base of the tongue (Fig.2 A&B). A chest venogram to evaluate for SVC obstruction was negative. A flexible laryngoscopy confirmed the presence of sublingual varices. The patient refused a colonoscopy, and during his hospitalization, he had no further episodes of gastrointestinal bleeding; his anemia improved, and he was discharged. He was instructed to follow up with gastroenterology for further workup of his anemia.
Discussion: DV is a rare entity and, when found, is most commonly caused by SVC obstruction. In our case, chest venogram was negative. Other rare causes of PEV are severe pulmonary hypertension, Behcet’s disease, complications with hemodialysis catheters, or mediastinal fibrosis. In our patient, it is most likely that he developed DV secondary to severe pulmonary hypertension in the setting of severe COPD, as chest and neck imaging was negative for SVC obstruction. There are currently no recommendations for the endoscopic management of DV, but treatment should be aimed at correcting the underlying cause. Other options, such as endoscopic band ligation, sclerotherapy, or balloon tamponade may temporize active DV bleeding. Although rare, gastroenterologists should be familiar with DV and perform a careful esophageal and oropharyngeal exam, especially in patients with underlying lung disease.
Disclosures:
Bianca Thakkar, DO1, Teresa Da Cunha, MD1, Rachael Hagen, DO2, Roopjeet K. Bath, MBBS3. P0542 - Pulmonary Hypertension and Downhill Varices: An Incidental Finding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Connecticut Health Center, Farmington, CT; 2University of Connecticut Health, Farmington, CT; 3UConn Health, Farmington, CT
Introduction: Esophageal varices are dilated submucosal esophageal veins connecting the portal and systemic circulation. Compared to distal esophageal varices, downhill varices (DV) are a rare entity and can occur in the middle and proximal esophagus. DV usually results from an obstruction of the superior vena cava (SVC). Incidental DVs are rare and require further workup. We describe a case of a patient who presented with shortness of breath and melena and was found to have DVs.
Case Description/Methods: An 80-year-old male with a history of chronic obstructive pulmonary disease, severe pulmonary hypertension, heart failure with reduced ejection fraction, and significant prior smoking history presented to the emergency room with shortness of breath and melena. He had a hemoglobin of 5.9 from a baseline of 9. After adequate resuscitation, an EGD was performed, which showed non-bleeding varices in the proximal third of the esophagus (Fig.1 A&B) and a vascular lesion on the base of the tongue (Fig.2 A&B). A chest venogram to evaluate for SVC obstruction was negative. A flexible laryngoscopy confirmed the presence of sublingual varices. The patient refused a colonoscopy, and during his hospitalization, he had no further episodes of gastrointestinal bleeding; his anemia improved, and he was discharged. He was instructed to follow up with gastroenterology for further workup of his anemia.
Discussion: DV is a rare entity and, when found, is most commonly caused by SVC obstruction. In our case, chest venogram was negative. Other rare causes of PEV are severe pulmonary hypertension, Behcet’s disease, complications with hemodialysis catheters, or mediastinal fibrosis. In our patient, it is most likely that he developed DV secondary to severe pulmonary hypertension in the setting of severe COPD, as chest and neck imaging was negative for SVC obstruction. There are currently no recommendations for the endoscopic management of DV, but treatment should be aimed at correcting the underlying cause. Other options, such as endoscopic band ligation, sclerotherapy, or balloon tamponade may temporize active DV bleeding. Although rare, gastroenterologists should be familiar with DV and perform a careful esophageal and oropharyngeal exam, especially in patients with underlying lung disease.
Figure: Figure 1 A and B. Upper endoscopy with proximal esophageal varices seen as various blebs with a diffuse distribution.
Figure 2 A and B. Upper endoscopy with vascular lesion seen at base of tongue, confirmed as sublingual varices on laryngoscopy.
Figure 2 A and B. Upper endoscopy with vascular lesion seen at base of tongue, confirmed as sublingual varices on laryngoscopy.
Disclosures:
Bianca Thakkar indicated no relevant financial relationships.
Teresa Da Cunha indicated no relevant financial relationships.
Rachael Hagen indicated no relevant financial relationships.
Roopjeet Bath indicated no relevant financial relationships.
Bianca Thakkar, DO1, Teresa Da Cunha, MD1, Rachael Hagen, DO2, Roopjeet K. Bath, MBBS3. P0542 - Pulmonary Hypertension and Downhill Varices: An Incidental Finding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
