Sunday Poster Session
Category: Esophagus
P0565 - Synchronous Oropharyngeal and Esophageal HPV-Associated Squamous Cell Carcinoma: A Call for Endoscopic Screening?
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Hamzah Shariff, MD
Thomas Jefferson University Hospital
Philadelphia, PA
Presenting Author(s)
Hamzah Shariff, MD1, Shiva Naidoo, MD2, Ghazal Ghafari, DO, MPH3, Jianhong Li, MD3, John Appiah, MD4, Gurkaramjit Khaira, MD5, Shaheen Jaisingh, 6, Danyall Saeed, 7, Umar Hayat, MD4, Raeva Mulloth, 7, Abhinav Goyal, MD5
1Thomas Jefferson University Hospital, Philadelphia, PA; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3Geisinger Health System, Danville, PA; 4Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 5Geisinger Community Medical Center, Scranton, PA; 6University of Pennsylvania, Philadelphia, PA; 7Geisinger Commonwealth School of Medicine, Scranton, PA
Introduction: Synchronous human papillomavirus (HPV)-mediated oropharyngeal squamous cell carcinoma (OSCC) and esophageal squamous cell carcinoma (ESCC) are rare. Due to this rarity, screening endoscopy isn't typically recommended. We present a case of HPV-mediated OSCC with melena, incidentally revealing ESCC as a second primary malignancy during esophagogastroduodenoscopy (EGD).
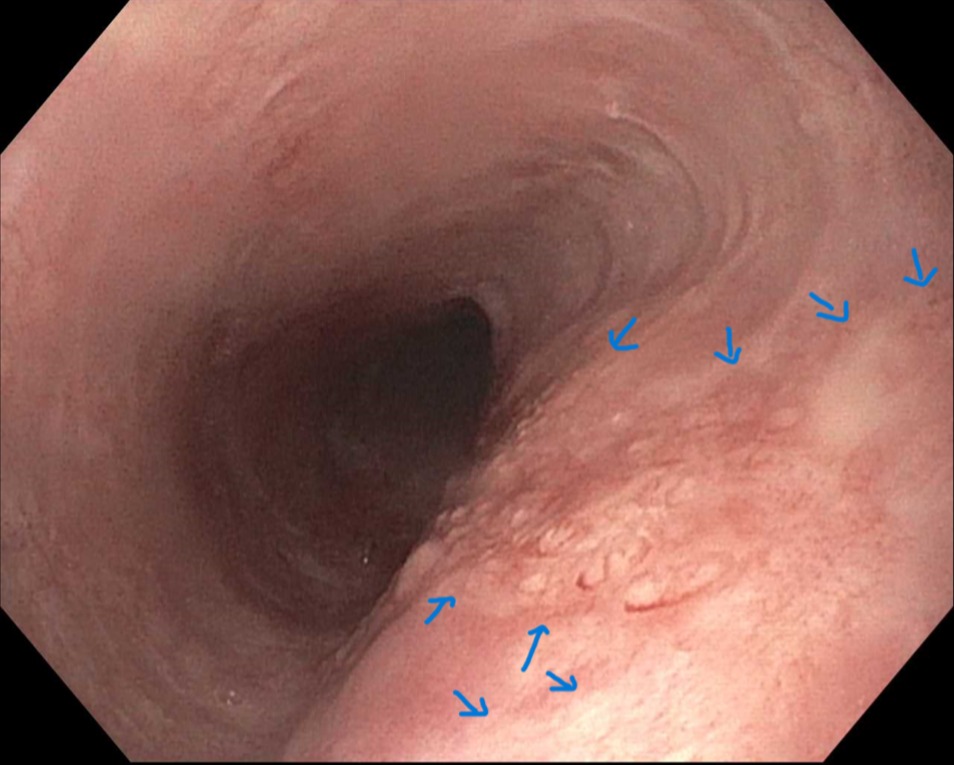
Case Description/Methods: A 67-year-old male with heavy tobacco use, compensated alcoholic cirrhosis, and recently diagnosed HPV-16 mediated SCC in the left palatine tonsil presented with black tarry stools. He was hemodynamically stable, but cachectic. Laboratory results showed a decrease in hemoglobin (13.8 from 18 g/dL), blood urea nitrogen of 28 mg/dL, INR of 1.07, and platelet count of 228. EGD revealed duodenal erosions without bleeding. An altered serpiginous vascular pattern was also incidentally noted in the middle esophagus at 35 cm from the incisors. Biopsies showed dysplastic squamous epithelium. Subsequent endoscopic mucosal resection (EMR) of this region was performed and revealed carcinoma in situ with positive resection margins. PET CT showed hypermetabolic activity in the left palatine tonsil and left level IB cervical lymph node. OSCC was treated with chemotherapy and radiation for 2 months. He underwent multiple EMRs and cryoablation for recurrent ESCC during surveillance endoscopies as he was deemed to be a poor surgical candidate.
Discussion: Upper endoscopy is a valuable tool for screening for second malignancy in the esophagus for confirmed head and neck SCC, but not typically recommended due to low diagnostic yield. However, our patient's EGD for melena incidentally detected synchronous ESCC with HPV-mediated OSCC. Moreover, the subtle vascular pattern changes noted at the time of endoscopy which aided early detection require thorough inspection and high index of suspicion. Interestingly, PET CT failed to detect ESCC despite endoscopic findings indicating low sensitivity. While the risk of ESCC as a second primary malignancy is lower in HPV-mediated than non-HPV-mediated OSCC, its diagnosis impacts prognosis negatively. Our case suggests the need for further study on endoscopic screening early detection of ESCC synchronous with HPV-mediated OSCC.
Disclosures:
Hamzah Shariff, MD1, Shiva Naidoo, MD2, Ghazal Ghafari, DO, MPH3, Jianhong Li, MD3, John Appiah, MD4, Gurkaramjit Khaira, MD5, Shaheen Jaisingh, 6, Danyall Saeed, 7, Umar Hayat, MD4, Raeva Mulloth, 7, Abhinav Goyal, MD5. P0565 - Synchronous Oropharyngeal and Esophageal HPV-Associated Squamous Cell Carcinoma: A Call for Endoscopic Screening?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Thomas Jefferson University Hospital, Philadelphia, PA; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3Geisinger Health System, Danville, PA; 4Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 5Geisinger Community Medical Center, Scranton, PA; 6University of Pennsylvania, Philadelphia, PA; 7Geisinger Commonwealth School of Medicine, Scranton, PA
Introduction: Synchronous human papillomavirus (HPV)-mediated oropharyngeal squamous cell carcinoma (OSCC) and esophageal squamous cell carcinoma (ESCC) are rare. Due to this rarity, screening endoscopy isn't typically recommended. We present a case of HPV-mediated OSCC with melena, incidentally revealing ESCC as a second primary malignancy during esophagogastroduodenoscopy (EGD).
Case Description/Methods: A 67-year-old male with heavy tobacco use, compensated alcoholic cirrhosis, and recently diagnosed HPV-16 mediated SCC in the left palatine tonsil presented with black tarry stools. He was hemodynamically stable, but cachectic. Laboratory results showed a decrease in hemoglobin (13.8 from 18 g/dL), blood urea nitrogen of 28 mg/dL, INR of 1.07, and platelet count of 228. EGD revealed duodenal erosions without bleeding. An altered serpiginous vascular pattern was also incidentally noted in the middle esophagus at 35 cm from the incisors. Biopsies showed dysplastic squamous epithelium. Subsequent endoscopic mucosal resection (EMR) of this region was performed and revealed carcinoma in situ with positive resection margins. PET CT showed hypermetabolic activity in the left palatine tonsil and left level IB cervical lymph node. OSCC was treated with chemotherapy and radiation for 2 months. He underwent multiple EMRs and cryoablation for recurrent ESCC during surveillance endoscopies as he was deemed to be a poor surgical candidate.
Discussion: Upper endoscopy is a valuable tool for screening for second malignancy in the esophagus for confirmed head and neck SCC, but not typically recommended due to low diagnostic yield. However, our patient's EGD for melena incidentally detected synchronous ESCC with HPV-mediated OSCC. Moreover, the subtle vascular pattern changes noted at the time of endoscopy which aided early detection require thorough inspection and high index of suspicion. Interestingly, PET CT failed to detect ESCC despite endoscopic findings indicating low sensitivity. While the risk of ESCC as a second primary malignancy is lower in HPV-mediated than non-HPV-mediated OSCC, its diagnosis impacts prognosis negatively. Our case suggests the need for further study on endoscopic screening early detection of ESCC synchronous with HPV-mediated OSCC.
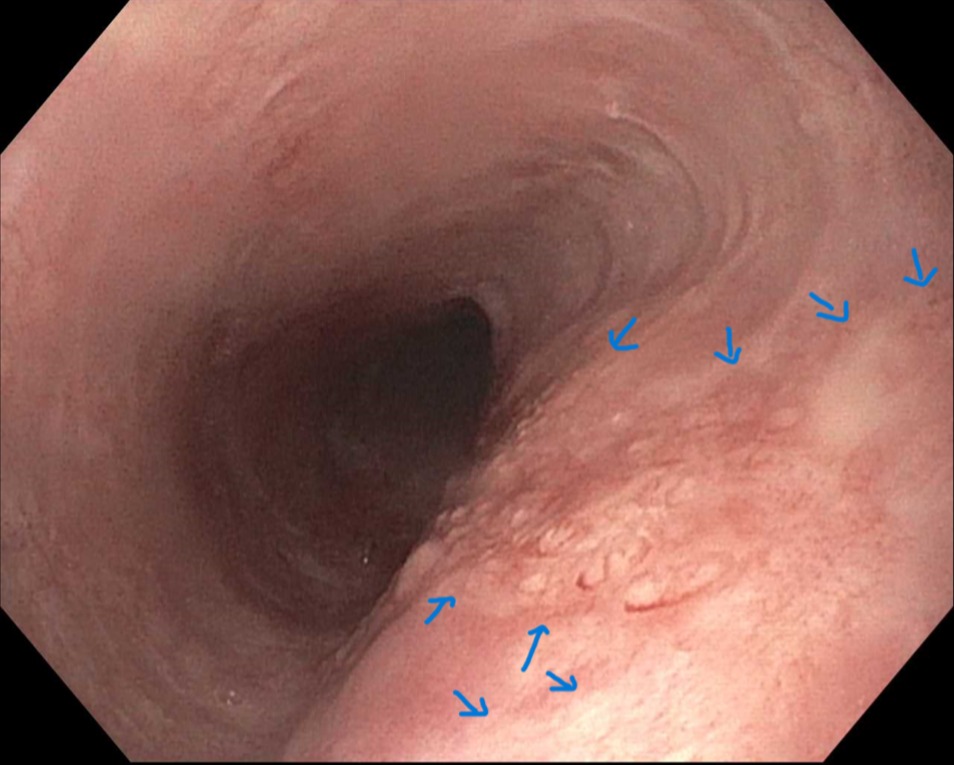
Figure: EGD of the middle esophagus with large mucosal erosion and serpiginous vasculature
Disclosures:
Hamzah Shariff indicated no relevant financial relationships.
Shiva Naidoo indicated no relevant financial relationships.
Ghazal Ghafari indicated no relevant financial relationships.
Jianhong Li indicated no relevant financial relationships.
John Appiah indicated no relevant financial relationships.
Gurkaramjit Khaira indicated no relevant financial relationships.
Shaheen Jaisingh indicated no relevant financial relationships.
Danyall Saeed indicated no relevant financial relationships.
Umar Hayat indicated no relevant financial relationships.
Raeva Mulloth indicated no relevant financial relationships.
Abhinav Goyal indicated no relevant financial relationships.
Hamzah Shariff, MD1, Shiva Naidoo, MD2, Ghazal Ghafari, DO, MPH3, Jianhong Li, MD3, John Appiah, MD4, Gurkaramjit Khaira, MD5, Shaheen Jaisingh, 6, Danyall Saeed, 7, Umar Hayat, MD4, Raeva Mulloth, 7, Abhinav Goyal, MD5. P0565 - Synchronous Oropharyngeal and Esophageal HPV-Associated Squamous Cell Carcinoma: A Call for Endoscopic Screening?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

