Sunday Poster Session
Category: Esophagus
P0566 - A Rare Case of CMV Esophagitis in a Patient With Follicular Lymphoma
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Shefali Amin, DO, MSEd
Geisinger Health System
Wilkes-Barre, PA
Presenting Author(s)
Shefali Amin, DO, MSEd1, Abishek Hariharan, MD2, Manish Shrestha, MD2, Vinita Yadav, DO2, Kelly Brenan-Rothschild, MD3, Parth Desai, DO2, Nirav Shah, MD2
1Geisinger Health System, Wilkes-Barre, PA; 2Reading Tower Health, Reading, PA; 3Reading Hospital - Tower Health, Reading, PA
Introduction: Cytomegalovirus (CMV) can infect any area of the gastrointestinal tract. CMV esophagitis most commonly occurs in immunocompromised patients, such as those with Human Immunodeficiency Virus (HIV) or on immunosuppressive therapy. We present the case of a patient with follicular lymphoma who developed CMV esophagitis shortly after starting chemotherapy
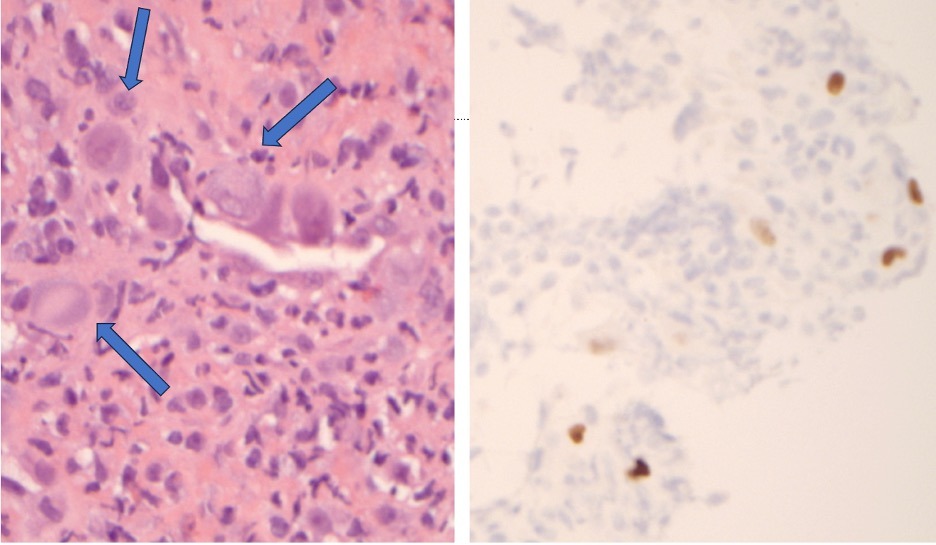
Case Description/Methods: A 66-year-old male patient with a history of stage IV follicular lymphoma presented due to a two-week history of painful oral lesions, odynophagia with solids and liquids, and a generalized pruritic rash. Further history revealed tenesmus, pain with defecation, and tender perianal region. He denied fever, chills, recent travel, or sick contacts. He was on chemotherapy with bendamustine and rituximab, last session two months prior; however, he did admit to noncompliance with his prophylactic acyclovir. He was hemodynamically stable on admission. Physical exam revealed erythematous oral mucosa with aphthous ulcers, a maculopapular rash with non-blanchable skin lesions on the trunk and proximal extremities, and tender perianal ulcers. Laboratory results showed an elevated creatinine of 2.03 mg/dL and mild leukopenia at 4300 x103/uL. There was initial concern for herpes simplex infection (HSV), and he was started on oral acyclovir. HIV, CMV, and Steven-Johnson syndrome, were other differentials also considered given risk of immunosuppression from recent bendamustine. Initial testing was negative for HSV and HIV. Further work up revealed his CD4 count was less than 35 and CMV quantitative PCR was elevated at 1285 IU/mL. His symptoms prompted an upper endoscopy, which showed posterior oropharynx ulcerations and confluent streaky ulcerations in the distal esophagus with surrounding erythema. At this time, he was switched to valganciclovir for treatment of CMV esophagitis. The diagnosis was confirmed by positive anti-CMV monoclonal antibody immunohistochemical staining of distal esophageal biopsies (Figure 1). At discharge, he was continued on oral valganciclovir 900mg twice daily for at least 3 weeks and follow-up with outpatient Infectious Disease.
Discussion: For immunocompromised patients presenting with persistent gastrointestinal symptoms, further investigation with endoscopy is warranted to reveal the underlying cause. CMV esophagitis is diagnosed by a combination of clinical history, endoscopic findings, and histologic features. The case highlights the importance of endoscopic evaluation to allow for proper treatment.
Disclosures:
Shefali Amin, DO, MSEd1, Abishek Hariharan, MD2, Manish Shrestha, MD2, Vinita Yadav, DO2, Kelly Brenan-Rothschild, MD3, Parth Desai, DO2, Nirav Shah, MD2. P0566 - A Rare Case of CMV Esophagitis in a Patient With Follicular Lymphoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Geisinger Health System, Wilkes-Barre, PA; 2Reading Tower Health, Reading, PA; 3Reading Hospital - Tower Health, Reading, PA
Introduction: Cytomegalovirus (CMV) can infect any area of the gastrointestinal tract. CMV esophagitis most commonly occurs in immunocompromised patients, such as those with Human Immunodeficiency Virus (HIV) or on immunosuppressive therapy. We present the case of a patient with follicular lymphoma who developed CMV esophagitis shortly after starting chemotherapy
Case Description/Methods: A 66-year-old male patient with a history of stage IV follicular lymphoma presented due to a two-week history of painful oral lesions, odynophagia with solids and liquids, and a generalized pruritic rash. Further history revealed tenesmus, pain with defecation, and tender perianal region. He denied fever, chills, recent travel, or sick contacts. He was on chemotherapy with bendamustine and rituximab, last session two months prior; however, he did admit to noncompliance with his prophylactic acyclovir. He was hemodynamically stable on admission. Physical exam revealed erythematous oral mucosa with aphthous ulcers, a maculopapular rash with non-blanchable skin lesions on the trunk and proximal extremities, and tender perianal ulcers. Laboratory results showed an elevated creatinine of 2.03 mg/dL and mild leukopenia at 4300 x103/uL. There was initial concern for herpes simplex infection (HSV), and he was started on oral acyclovir. HIV, CMV, and Steven-Johnson syndrome, were other differentials also considered given risk of immunosuppression from recent bendamustine. Initial testing was negative for HSV and HIV. Further work up revealed his CD4 count was less than 35 and CMV quantitative PCR was elevated at 1285 IU/mL. His symptoms prompted an upper endoscopy, which showed posterior oropharynx ulcerations and confluent streaky ulcerations in the distal esophagus with surrounding erythema. At this time, he was switched to valganciclovir for treatment of CMV esophagitis. The diagnosis was confirmed by positive anti-CMV monoclonal antibody immunohistochemical staining of distal esophageal biopsies (Figure 1). At discharge, he was continued on oral valganciclovir 900mg twice daily for at least 3 weeks and follow-up with outpatient Infectious Disease.
Discussion: For immunocompromised patients presenting with persistent gastrointestinal symptoms, further investigation with endoscopy is warranted to reveal the underlying cause. CMV esophagitis is diagnosed by a combination of clinical history, endoscopic findings, and histologic features. The case highlights the importance of endoscopic evaluation to allow for proper treatment.
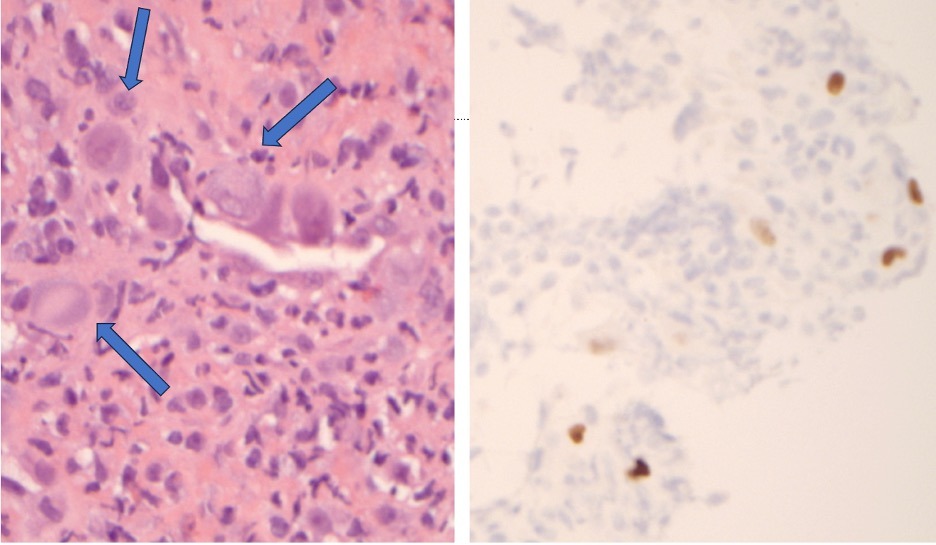
Figure: Figure 1: A) High power of the biopsy of esophageal ulcer bed showing endothelial cells with intranuclear and basophilic intracytoplasmic inclusions, morphologically consistent with cytomegalovirus (CMV); B) confirmed by CMV immunohistochemistry
Disclosures:
Shefali Amin indicated no relevant financial relationships.
Abishek Hariharan indicated no relevant financial relationships.
Manish Shrestha indicated no relevant financial relationships.
Vinita Yadav indicated no relevant financial relationships.
Kelly Brenan-Rothschild indicated no relevant financial relationships.
Parth Desai indicated no relevant financial relationships.
Nirav Shah indicated no relevant financial relationships.
Shefali Amin, DO, MSEd1, Abishek Hariharan, MD2, Manish Shrestha, MD2, Vinita Yadav, DO2, Kelly Brenan-Rothschild, MD3, Parth Desai, DO2, Nirav Shah, MD2. P0566 - A Rare Case of CMV Esophagitis in a Patient With Follicular Lymphoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
