Sunday Poster Session
Category: Esophagus
P0570 - Clinical Management and Outcomes in Esophageal Leukoplakia: A Case Series
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Rohini Maddigunta, BS
Cooper Medical School of Rowan University
Camden, NJ
Presenting Author(s)
Fariha Hasan, MD1, Rohini Maddigunta, BS2, Krysta Contino, MD3, Christina Tofani, MD, FACG4
1Cooper University Hospital, Philadelphia, PA; 2Cooper Medical School of Rowan University, Camden, NJ; 3Digestive Health Institute at Cooper University Hospital, Mount Laurel, NJ; 4Digestive Health Institute at Cooper University Hospital, Camden, NJ
Introduction: Esophageal leukoplakia is a rare condition predominantly affecting the middle to distal esophagus, characterized by hyperkeratotic white plaques on the esophageal mucosa. Patients often present with nonspecific symptoms such as dysphagia, odynophagia, and a globus sensation. Diagnosis relies heavily on esophagogastroduodenoscopy (EGD). Although benign, esophageal leukoplakia is classified as a premalignant lesion due to its potential to progress into esophageal squamous cell carcinoma (ESCC), necessitating meticulous clinical management. This report presents two cases of esophageal leukoplakia, elucidating their clinical courses and management strategies.
Case Description/Methods: Case 1
A 77-year-old male with a longstanding history of esophageal leukoplakia presented for evaluation of intermittent dysphagia. He had previously undergone biannual upper endoscopies with biopsies consistently showing hyperkeratosis, parakeratosis, and epidermoid metaplasia without evidence of dysplasia. He undergoes EGDs with brush cytology and biopsies biannually. His most recent EGD revealed leukoplakia in the distal esophagus, from 31 to 38 cm from the incisors, with circumferential involvement from 34 to 38 cm and several tongues extending from 31 to 34 cm. A repeat endoscopy is scheduled in six months, with the continuation of Omeprazole twice a day.
Case 2
A 60-year-old female with a history of a duodenal switch presented for evaluation of chronic abdominal pain with dyspepsia. EGD with biopsy results showed esophageal squamous mucosa with epidermoid metaplasia at 38 cm. A subsequent EGD two months later revealed squamous epithelium with parakeratosis and focal epidermoid metaplasia from 28-36 cm. The patient was advised to continue omeprazole 40 mg orally twice daily and to follow up for surveillance EGD. Unfortunately, she has been lost to follow-up.
Discussion: Approximately 5-10% of esophageal leukoplakia cases progress to ESCC, underscoring the importance of regular follow-ups and interval EGDs, as highlighted by the presented patient reports. Given the rarity of esophageal leukoplakia, specific guidelines for EGD frequency are lacking. Surveillance should be tailored to individual patient risk factors and clinical judgment, with most case reports recommending intervals of 3 to 12 months. Consistent monitoring and timely intervention can significantly enhance patient outcomes by preventing progression to invasive malignancy and ensuring optimal management of this rare condition.
Disclosures:
Fariha Hasan, MD1, Rohini Maddigunta, BS2, Krysta Contino, MD3, Christina Tofani, MD, FACG4. P0570 - Clinical Management and Outcomes in Esophageal Leukoplakia: A Case Series, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cooper University Hospital, Philadelphia, PA; 2Cooper Medical School of Rowan University, Camden, NJ; 3Digestive Health Institute at Cooper University Hospital, Mount Laurel, NJ; 4Digestive Health Institute at Cooper University Hospital, Camden, NJ
Introduction: Esophageal leukoplakia is a rare condition predominantly affecting the middle to distal esophagus, characterized by hyperkeratotic white plaques on the esophageal mucosa. Patients often present with nonspecific symptoms such as dysphagia, odynophagia, and a globus sensation. Diagnosis relies heavily on esophagogastroduodenoscopy (EGD). Although benign, esophageal leukoplakia is classified as a premalignant lesion due to its potential to progress into esophageal squamous cell carcinoma (ESCC), necessitating meticulous clinical management. This report presents two cases of esophageal leukoplakia, elucidating their clinical courses and management strategies.
Case Description/Methods: Case 1
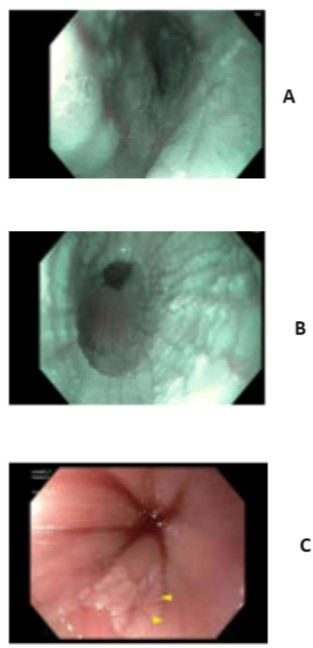
A 77-year-old male with a longstanding history of esophageal leukoplakia presented for evaluation of intermittent dysphagia. He had previously undergone biannual upper endoscopies with biopsies consistently showing hyperkeratosis, parakeratosis, and epidermoid metaplasia without evidence of dysplasia. He undergoes EGDs with brush cytology and biopsies biannually. His most recent EGD revealed leukoplakia in the distal esophagus, from 31 to 38 cm from the incisors, with circumferential involvement from 34 to 38 cm and several tongues extending from 31 to 34 cm. A repeat endoscopy is scheduled in six months, with the continuation of Omeprazole twice a day.
Case 2
A 60-year-old female with a history of a duodenal switch presented for evaluation of chronic abdominal pain with dyspepsia. EGD with biopsy results showed esophageal squamous mucosa with epidermoid metaplasia at 38 cm. A subsequent EGD two months later revealed squamous epithelium with parakeratosis and focal epidermoid metaplasia from 28-36 cm. The patient was advised to continue omeprazole 40 mg orally twice daily and to follow up for surveillance EGD. Unfortunately, she has been lost to follow-up.
Discussion: Approximately 5-10% of esophageal leukoplakia cases progress to ESCC, underscoring the importance of regular follow-ups and interval EGDs, as highlighted by the presented patient reports. Given the rarity of esophageal leukoplakia, specific guidelines for EGD frequency are lacking. Surveillance should be tailored to individual patient risk factors and clinical judgment, with most case reports recommending intervals of 3 to 12 months. Consistent monitoring and timely intervention can significantly enhance patient outcomes by preventing progression to invasive malignancy and ensuring optimal management of this rare condition.
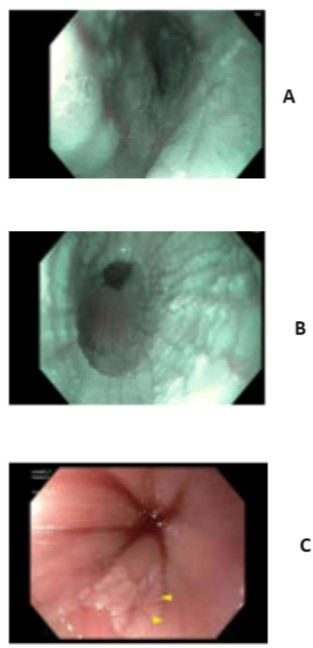
Figure: Figure A-EGD Image of Case 1 Esophageal Leukoplakia Plaque 34-38 cm, Figure B EGD Image Case 1 Esophageal Leukoplakia Plaque Middle Third of the Esophagus, Figure C EGD Image Case 2 Esophageal Leukoplakia Plaque at 38 cm
Disclosures:
Fariha Hasan indicated no relevant financial relationships.
Rohini Maddigunta indicated no relevant financial relationships.
Krysta Contino indicated no relevant financial relationships.
Christina Tofani indicated no relevant financial relationships.
Fariha Hasan, MD1, Rohini Maddigunta, BS2, Krysta Contino, MD3, Christina Tofani, MD, FACG4. P0570 - Clinical Management and Outcomes in Esophageal Leukoplakia: A Case Series, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
