Sunday Poster Session
Category: Esophagus
P0595 - A Tough Diagnosis to Swallow: Management of Coexisting Achalasia and Esophageal Varices with Transjugular Intrahepatic Porto-Systemic Shunting
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Heather Gosnell, DO
University of South Florida Morsani College of Medicine
Tampa, FL
Presenting Author(s)
Heather Gosnell, DO1, Scott Manski, MD2, Charles Cavalaris, MD1, Shreya Narayanan, MD2
1University of South Florida Morsani College of Medicine, Tampa, FL; 2University of South Florida, Tampa, FL
Introduction: Concomitant achalasia and esophageal varices (EV) present a unique challenge in the co-management of these conditions. Here we present a case of achalasia and gastroesophageal varices requiring transjugular intrahepatic portosystemic shunting (TIPS) for variceal bleeding.
Case Description/Methods: A 69-year-old man with cirrhosis due to metabolic dysfunction and alcohol associated liver disease with ascites and type 1 esophagogastric varices (GOV1) was admitted for dysphagia and weight loss. Esophagram showed bird beaking of the distal esophagus. Follow up EGD revealed a significantly tortuous and dilated esophagus, large EV, and GOV1. The patient was diagnosed with achalasia based on these findings but definitive diagnosis with esophageal manometry was deferred because of EV. EUS was also completed to rule out pseudoachalasia.
The patient was readmitted months later with melena with acute anemia and aspiration pneumonia. EGD showed a grossly tortuous and dilated esophagus with copious food debris without blood. The debris was extracted and upon advancement of the endoscope, blood was found throughout the stomach with GOV1 with fibrin cap seen on retroflexed view. Banding was not performed due to difficulty navigating the esophagus and positioning of the varix. The patient underwent TIPS with reduction in portal pressures and cessation of bleeding.
For nutritional optimization in the face of achalasia and with ascites, a nasoduodenal feeding tube was placed. After multidisciplinary discussion, the patient is planned for repeat EGD to reassess EV. Pending eradication, EndoFlip may be performed to confirm the achalasia diagnosis. Subsequent management options include esophageal Botox injections versus definitive surgical management at the time of or after liver transplant.
Discussion: This case presents a multifactorial challenge in managing bleeding varices with bleeding and achalasia with secondary dysphagia, aspiration, and malnutrition. Reported cases of achalasia and EV have been treated with Botox injection, pneumatic dilation, POEM, Heller myotomy, or a combination thereof. Management also involves optimizing nutrition to mitigate further decompensation and complication, which in this patient is further complicated by the presence of ascites.
Disclosures:
Heather Gosnell, DO1, Scott Manski, MD2, Charles Cavalaris, MD1, Shreya Narayanan, MD2. P0595 - A Tough Diagnosis to Swallow: Management of Coexisting Achalasia and Esophageal Varices with Transjugular Intrahepatic Porto-Systemic Shunting, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of South Florida Morsani College of Medicine, Tampa, FL; 2University of South Florida, Tampa, FL
Introduction: Concomitant achalasia and esophageal varices (EV) present a unique challenge in the co-management of these conditions. Here we present a case of achalasia and gastroesophageal varices requiring transjugular intrahepatic portosystemic shunting (TIPS) for variceal bleeding.
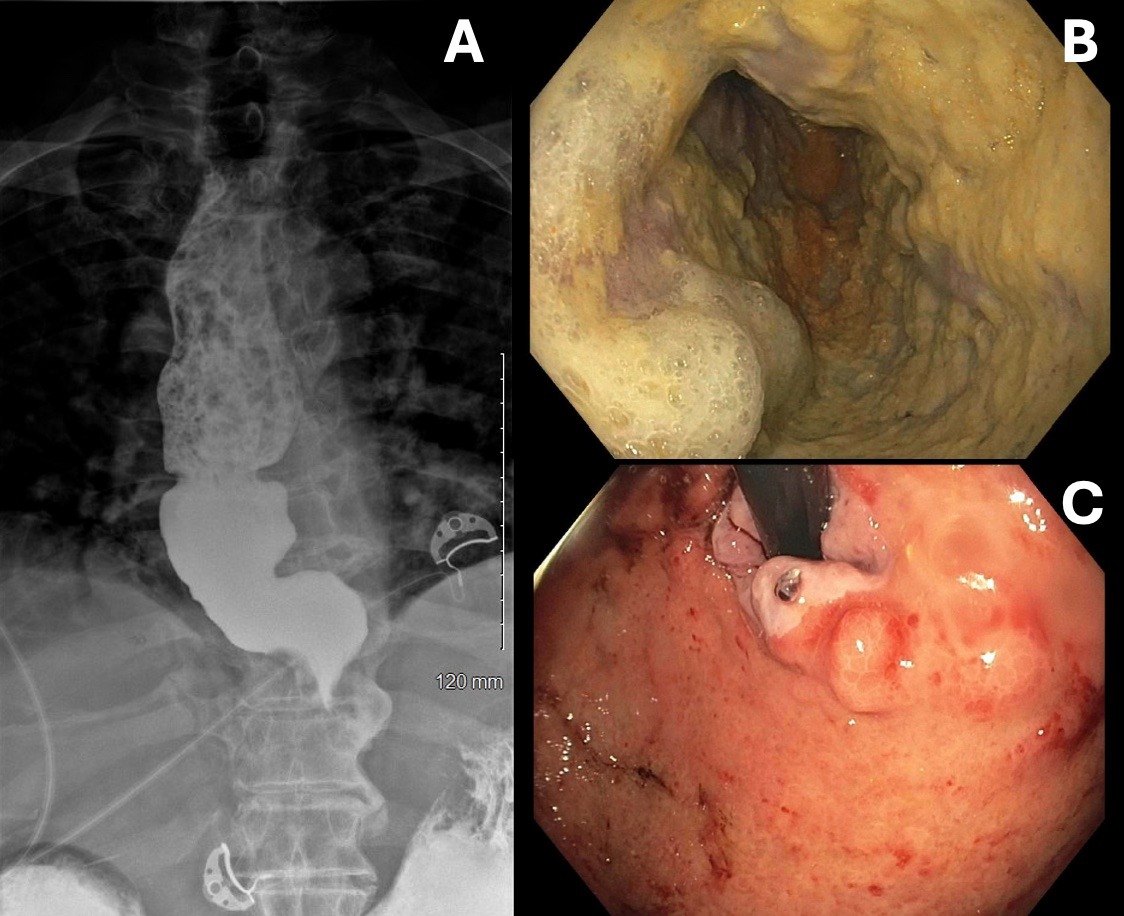
Case Description/Methods: A 69-year-old man with cirrhosis due to metabolic dysfunction and alcohol associated liver disease with ascites and type 1 esophagogastric varices (GOV1) was admitted for dysphagia and weight loss. Esophagram showed bird beaking of the distal esophagus. Follow up EGD revealed a significantly tortuous and dilated esophagus, large EV, and GOV1. The patient was diagnosed with achalasia based on these findings but definitive diagnosis with esophageal manometry was deferred because of EV. EUS was also completed to rule out pseudoachalasia.
The patient was readmitted months later with melena with acute anemia and aspiration pneumonia. EGD showed a grossly tortuous and dilated esophagus with copious food debris without blood. The debris was extracted and upon advancement of the endoscope, blood was found throughout the stomach with GOV1 with fibrin cap seen on retroflexed view. Banding was not performed due to difficulty navigating the esophagus and positioning of the varix. The patient underwent TIPS with reduction in portal pressures and cessation of bleeding.
For nutritional optimization in the face of achalasia and with ascites, a nasoduodenal feeding tube was placed. After multidisciplinary discussion, the patient is planned for repeat EGD to reassess EV. Pending eradication, EndoFlip may be performed to confirm the achalasia diagnosis. Subsequent management options include esophageal Botox injections versus definitive surgical management at the time of or after liver transplant.
Discussion: This case presents a multifactorial challenge in managing bleeding varices with bleeding and achalasia with secondary dysphagia, aspiration, and malnutrition. Reported cases of achalasia and EV have been treated with Botox injection, pneumatic dilation, POEM, Heller myotomy, or a combination thereof. Management also involves optimizing nutrition to mitigate further decompensation and complication, which in this patient is further complicated by the presence of ascites.
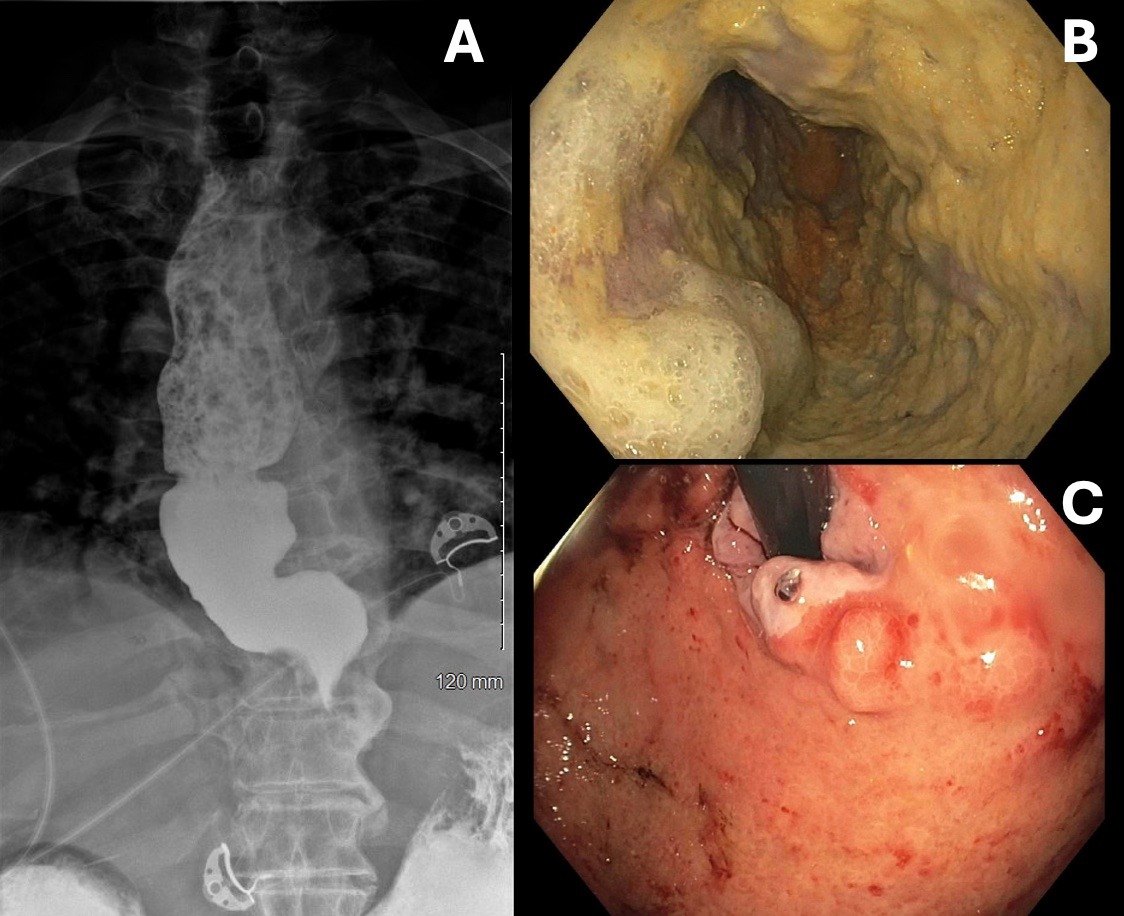
Figure: Figure 1: (1A) Barium esophagram with classic “bird beak” appearance of distal esophagus. (1B) Severely dilated mid esophagus with food debris and large esophageal varices. (1C) Retroflexed view of a gastroesophageal varix (GOV) type 1 with fibrin cap.
Disclosures:
Heather Gosnell indicated no relevant financial relationships.
Scott Manski indicated no relevant financial relationships.
Charles Cavalaris indicated no relevant financial relationships.
Shreya Narayanan indicated no relevant financial relationships.
Heather Gosnell, DO1, Scott Manski, MD2, Charles Cavalaris, MD1, Shreya Narayanan, MD2. P0595 - A Tough Diagnosis to Swallow: Management of Coexisting Achalasia and Esophageal Varices with Transjugular Intrahepatic Porto-Systemic Shunting, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
