Sunday Poster Session
Category: Esophagus
P0596 - Type B Aortic Dissection as the Cause of Esophageal Necrosis Leading to Severe Gastrointestinal Bleeding
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Daniel A. Guifarro, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Daniel A. Guifarro, MD, Alejandro Nieto Dominguez, MD, Seema Gandhi, MD
John H. Stroger, Jr. Hospital of Cook County, Chicago, IL
Introduction: Acute esophageal necrosis is a rare condition that presents due to ischemia leading to necrotizing esophagitis. Clinical presentation may vary, but it is usually seen in older males with multiple comorbidities and signs of upper gastrointestinal (GI) bleeding. It is a rare cause of upper GI bleeding, having an incidence of 0.01-0.28% of patients who undergo an upper endoscopy; in rare cases, an aortic dissection has been described as the direct cause.
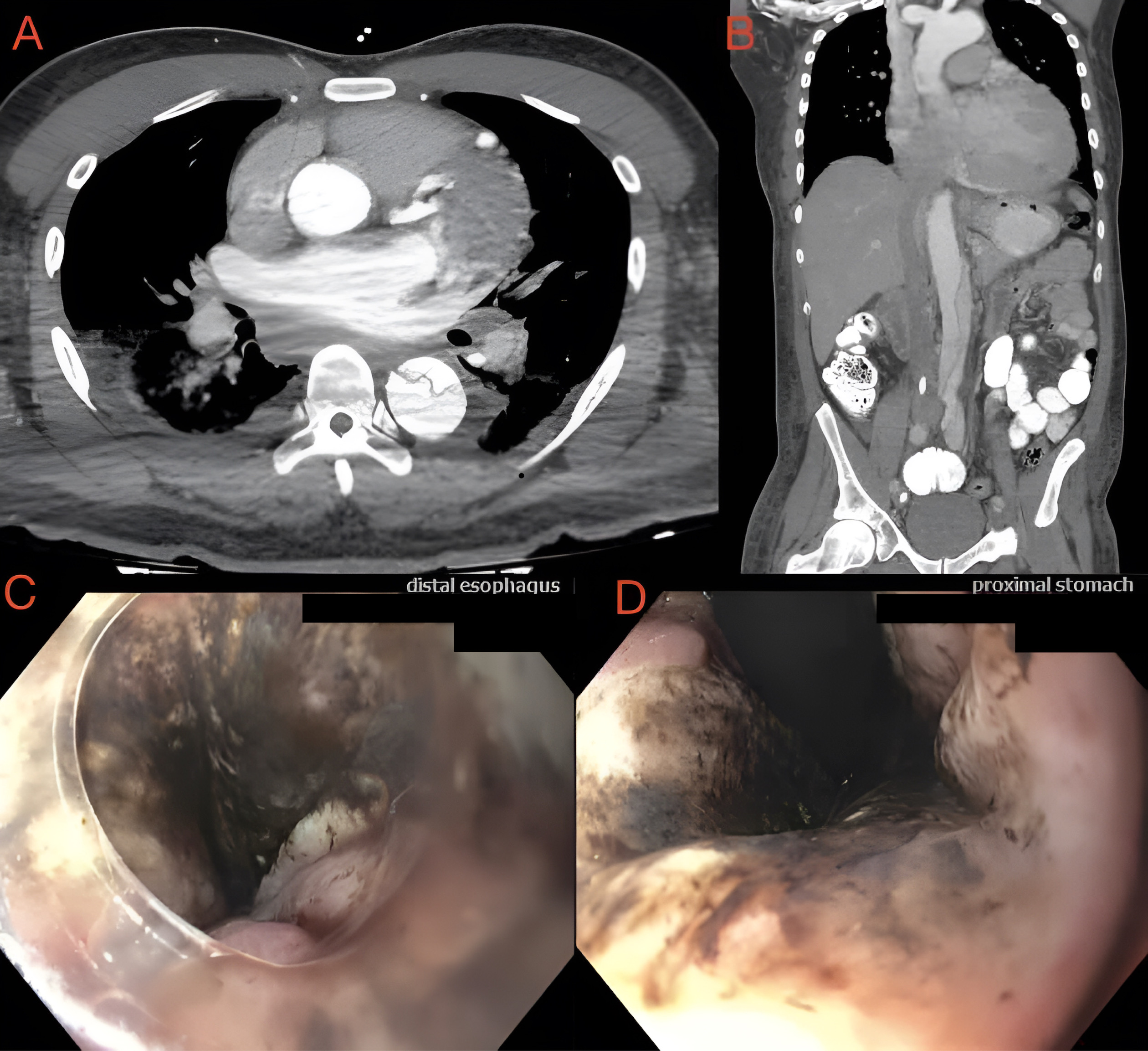
Case Description/Methods: A 47-year-old male with a history of uncontrolled Hypertension, multiple cerebrovascular accidents, chronic kidney disease, and a recent hemorrhagic stroke, presented to the emergency department with lower back pain and severe headache that started the day of admission. His blood pressure was 220/110 mmHg, laboratory exams showed a hemoglobin of 10.8 g/dL, BUN: 54 mg/dL, creatinine: 6.1 mg/dL; no other significant derangements were noted. A CT of the chest, abdomen, and pelvis with IV contrast was done, showing an acute Stanford type B dissection of the entire descending aorta, extending into the bilateral iliac and femoral arteries, and an intramural hematoma of the left subclavian artery. The patient was treated with nicardipine and esmolol drips for tight blood pressure control. He developed altered mental status and desaturation to 88% suspicious for aspiration; dark blood in the oral cavity was noted in addition to a hemoglobin drop to 6.9 g/dL, he was intubated for airway protection. An upper endoscopy was done, revealing circumferential mucosal blackening in the distal esophagus and gastric junction concerning for necrotizing esophagitis, mucosal pallor in the proximal stomach, a clot in the fundus, and a small Forrest III ulcer in the duodenal bulb; all findings were likely ischemic due to the presentation. Surgical interventions were deferred by cardiothoracic surgery, and aggressive blood pressure control was recommended with a goal of systolic blood pressure < 140mmHg. Treatment with esmolol and nicardipine continued achieving the goal, the patient did not have any recurrence of the bleeding and the hemoglobin continued to uptrend.
Discussion: Type B Aortic dissection has been rarely described as a cause of esophageal necrosis due to impaired blood flow of the aortic branches due to thrombotic occlusion of the false lumen, leading to ischemia. Treatment is normally conservative, with surgical interventions warranted in patients with complications such as perforation and persistence of bleeding.
Disclosures:
Daniel A. Guifarro, MD, Alejandro Nieto Dominguez, MD, Seema Gandhi, MD. P0596 - Type B Aortic Dissection as the Cause of Esophageal Necrosis Leading to Severe Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
John H. Stroger, Jr. Hospital of Cook County, Chicago, IL
Introduction: Acute esophageal necrosis is a rare condition that presents due to ischemia leading to necrotizing esophagitis. Clinical presentation may vary, but it is usually seen in older males with multiple comorbidities and signs of upper gastrointestinal (GI) bleeding. It is a rare cause of upper GI bleeding, having an incidence of 0.01-0.28% of patients who undergo an upper endoscopy; in rare cases, an aortic dissection has been described as the direct cause.
Case Description/Methods: A 47-year-old male with a history of uncontrolled Hypertension, multiple cerebrovascular accidents, chronic kidney disease, and a recent hemorrhagic stroke, presented to the emergency department with lower back pain and severe headache that started the day of admission. His blood pressure was 220/110 mmHg, laboratory exams showed a hemoglobin of 10.8 g/dL, BUN: 54 mg/dL, creatinine: 6.1 mg/dL; no other significant derangements were noted. A CT of the chest, abdomen, and pelvis with IV contrast was done, showing an acute Stanford type B dissection of the entire descending aorta, extending into the bilateral iliac and femoral arteries, and an intramural hematoma of the left subclavian artery. The patient was treated with nicardipine and esmolol drips for tight blood pressure control. He developed altered mental status and desaturation to 88% suspicious for aspiration; dark blood in the oral cavity was noted in addition to a hemoglobin drop to 6.9 g/dL, he was intubated for airway protection. An upper endoscopy was done, revealing circumferential mucosal blackening in the distal esophagus and gastric junction concerning for necrotizing esophagitis, mucosal pallor in the proximal stomach, a clot in the fundus, and a small Forrest III ulcer in the duodenal bulb; all findings were likely ischemic due to the presentation. Surgical interventions were deferred by cardiothoracic surgery, and aggressive blood pressure control was recommended with a goal of systolic blood pressure < 140mmHg. Treatment with esmolol and nicardipine continued achieving the goal, the patient did not have any recurrence of the bleeding and the hemoglobin continued to uptrend.
Discussion: Type B Aortic dissection has been rarely described as a cause of esophageal necrosis due to impaired blood flow of the aortic branches due to thrombotic occlusion of the false lumen, leading to ischemia. Treatment is normally conservative, with surgical interventions warranted in patients with complications such as perforation and persistence of bleeding.
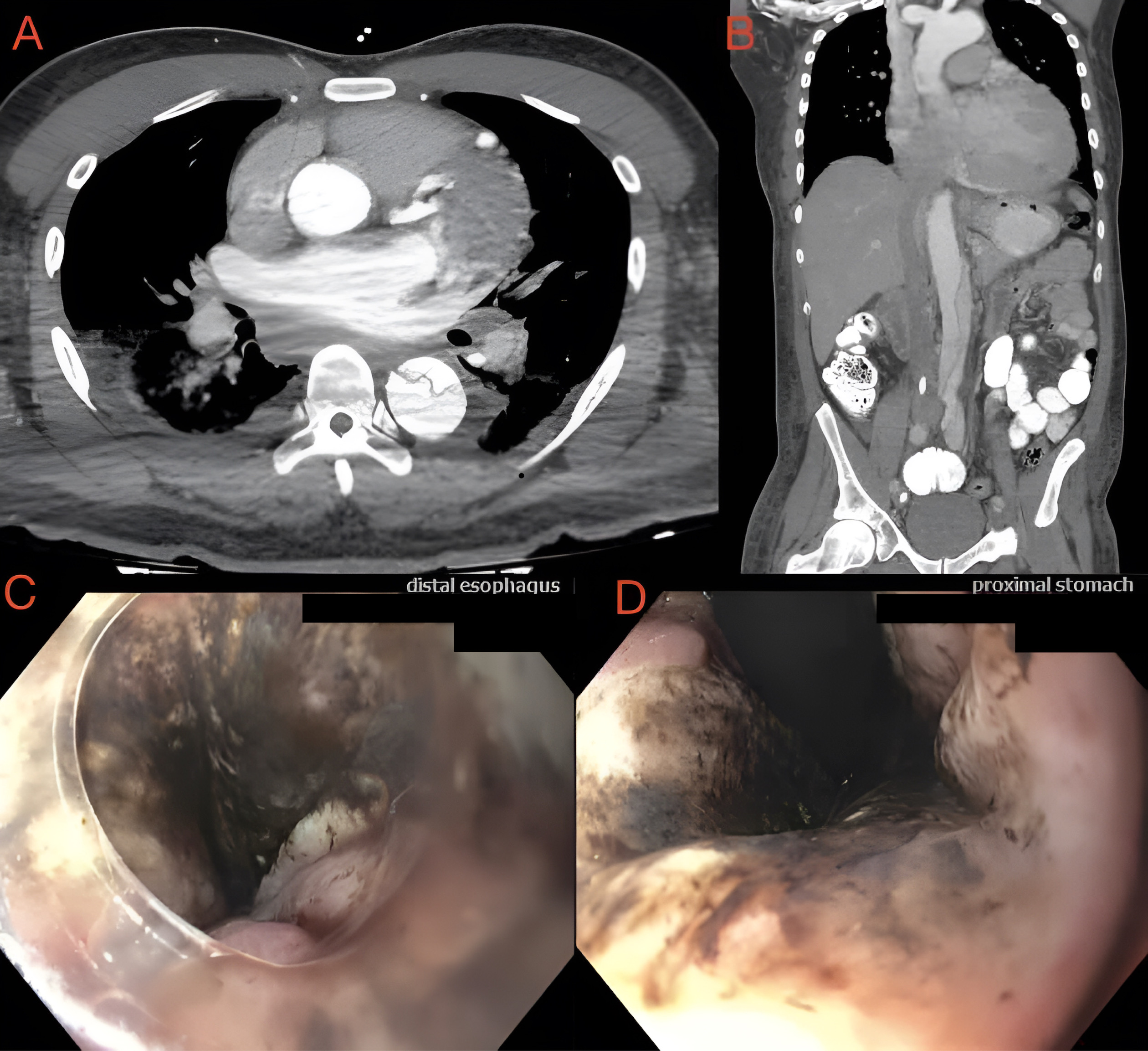
Figure: A and B: Aortic dissection seen progressing from descending thoracic aorta into the abdominal aorta.
C and D: Circumferential blackened esophageal mucosa related to necrotizing esophagitis in the distal esophagus and gastroesophageal junction.
C and D: Circumferential blackened esophageal mucosa related to necrotizing esophagitis in the distal esophagus and gastroesophageal junction.
Disclosures:
Daniel Guifarro indicated no relevant financial relationships.
Alejandro Nieto Dominguez indicated no relevant financial relationships.
Seema Gandhi indicated no relevant financial relationships.
Daniel A. Guifarro, MD, Alejandro Nieto Dominguez, MD, Seema Gandhi, MD. P0596 - Type B Aortic Dissection as the Cause of Esophageal Necrosis Leading to Severe Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
