Sunday Poster Session
Category: Esophagus
P0601 - CMV Esophagitis Presenting as Severe Anemia in an Asymptomatic, Immunocompetent Individual
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Joshua Freeman, DO
Swedish Covenant Hospital
Chicago, IL
Presenting Author(s)
Joshua Freeman, DO, Andrew Moore, MD
Swedish Covenant Hospital, Chicago, IL
Introduction: Cytomegalovirus (CMV) is a virus that infects a large percentage of the population. It lays dormant and reactivates in many organs, including the GI tract. Within which, it most commonly it affects the colon, and then the esophagus. Reactivation is more likely seen in immunosuppressed individuals; only a handful of cases have been reported in immunocompetent individuals. We present a case of CMV esophagitis, causing severe anemia in an immunocompetent host who displayed no classic symptoms.
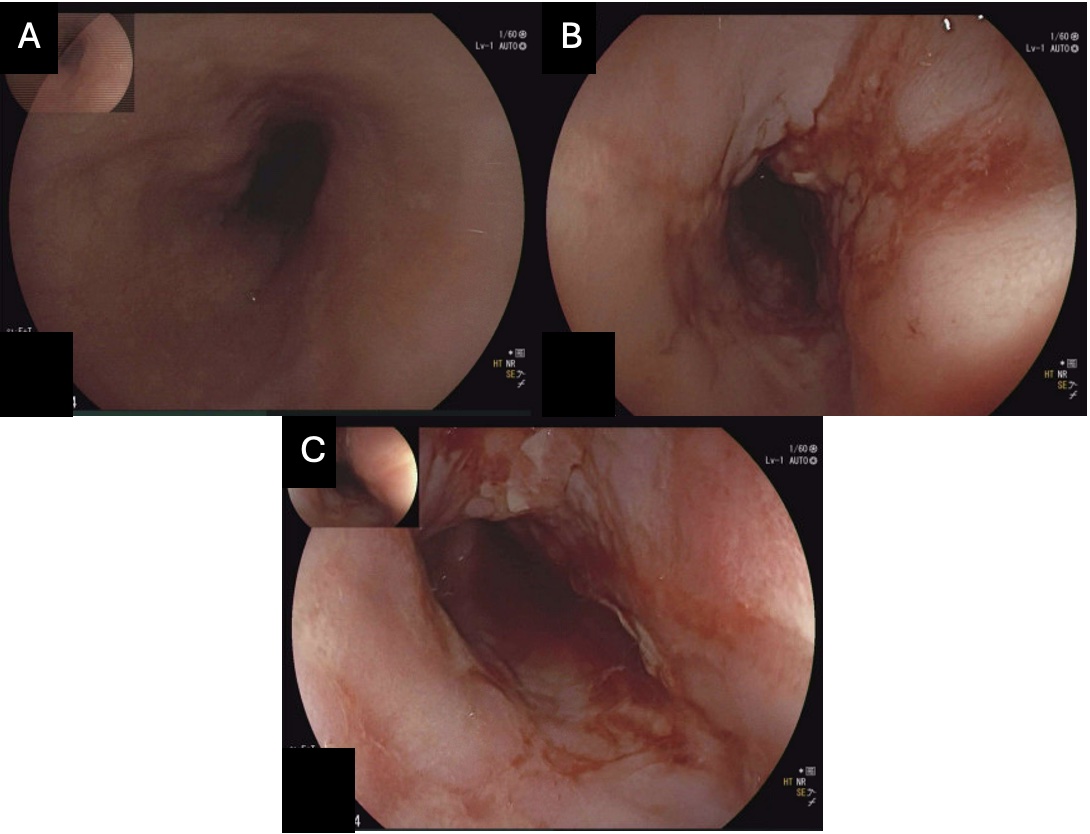
Case Description/Methods: 50 year old male with a history of depression and anxiety, presented to the ED with 1 day history of right arm and hand paresthesias. Initial vitals were significant for sinus tachycardia with heart rate of 108 and he was afebrile. Labs were significant for severe microcytic anemia with hemoglobin of 4.3, MCV 60.5, iron of 9 and ferritin of 2.0. WBC count was unremarkable. He had no signs of active bleeding and denied hematochezia or melena. Denied any use of blood thinners, NSAIDs or alcohol. He was transfused 3 units of red blood cells and given IV iron. Upper and lower endoscopies were performed. Upper endoscopy was significant for Grade D esophagitis with bleeding and showed congested, erythematous, eroded, friable, nodular texture changed mucosa in the esophagus. Biopsies were taken and he was discharged while awaiting results. Pathology showed squamocolumnar junctional mucosa with ulcer and CMV inclusions. He was called back to the hospital for treatment with IV ganciclovir for 4 days and discharged on oral valganciclovir for 16 additional days, along with PPI. HIV, hepatitis B & C testing were negative. He had no other immunocompromising conditions. Repeat EGD 3 months later showed improving esophagitis with no evidence of bleeding.
Discussion: Most often, patients with CMV esophagitis will present with odynophagia, dysphagia, nausea/vomiting and GERD. In our case, he did not display these symptoms and was immunocompetent. This case report serves to be one of the first reported case of severe occult anemia related to CMV esophagitis in an immunocompetent patient without classic symptoms. Primary CMV infection is known to cause hemolytic anemia. Severe reactivation CMV colitis/esophagitis can cause massive GI bleeds related to perforation. It is rare to see patients presenting with only anemia due to occult bleeding without any classic symptoms of esophagitis. Treatment requires IV anti-viral therapy with ganciclovir.
Disclosures:
Joshua Freeman, DO, Andrew Moore, MD. P0601 - CMV Esophagitis Presenting as Severe Anemia in an Asymptomatic, Immunocompetent Individual, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Swedish Covenant Hospital, Chicago, IL
Introduction: Cytomegalovirus (CMV) is a virus that infects a large percentage of the population. It lays dormant and reactivates in many organs, including the GI tract. Within which, it most commonly it affects the colon, and then the esophagus. Reactivation is more likely seen in immunosuppressed individuals; only a handful of cases have been reported in immunocompetent individuals. We present a case of CMV esophagitis, causing severe anemia in an immunocompetent host who displayed no classic symptoms.
Case Description/Methods: 50 year old male with a history of depression and anxiety, presented to the ED with 1 day history of right arm and hand paresthesias. Initial vitals were significant for sinus tachycardia with heart rate of 108 and he was afebrile. Labs were significant for severe microcytic anemia with hemoglobin of 4.3, MCV 60.5, iron of 9 and ferritin of 2.0. WBC count was unremarkable. He had no signs of active bleeding and denied hematochezia or melena. Denied any use of blood thinners, NSAIDs or alcohol. He was transfused 3 units of red blood cells and given IV iron. Upper and lower endoscopies were performed. Upper endoscopy was significant for Grade D esophagitis with bleeding and showed congested, erythematous, eroded, friable, nodular texture changed mucosa in the esophagus. Biopsies were taken and he was discharged while awaiting results. Pathology showed squamocolumnar junctional mucosa with ulcer and CMV inclusions. He was called back to the hospital for treatment with IV ganciclovir for 4 days and discharged on oral valganciclovir for 16 additional days, along with PPI. HIV, hepatitis B & C testing were negative. He had no other immunocompromising conditions. Repeat EGD 3 months later showed improving esophagitis with no evidence of bleeding.
Discussion: Most often, patients with CMV esophagitis will present with odynophagia, dysphagia, nausea/vomiting and GERD. In our case, he did not display these symptoms and was immunocompetent. This case report serves to be one of the first reported case of severe occult anemia related to CMV esophagitis in an immunocompetent patient without classic symptoms. Primary CMV infection is known to cause hemolytic anemia. Severe reactivation CMV colitis/esophagitis can cause massive GI bleeds related to perforation. It is rare to see patients presenting with only anemia due to occult bleeding without any classic symptoms of esophagitis. Treatment requires IV anti-viral therapy with ganciclovir.
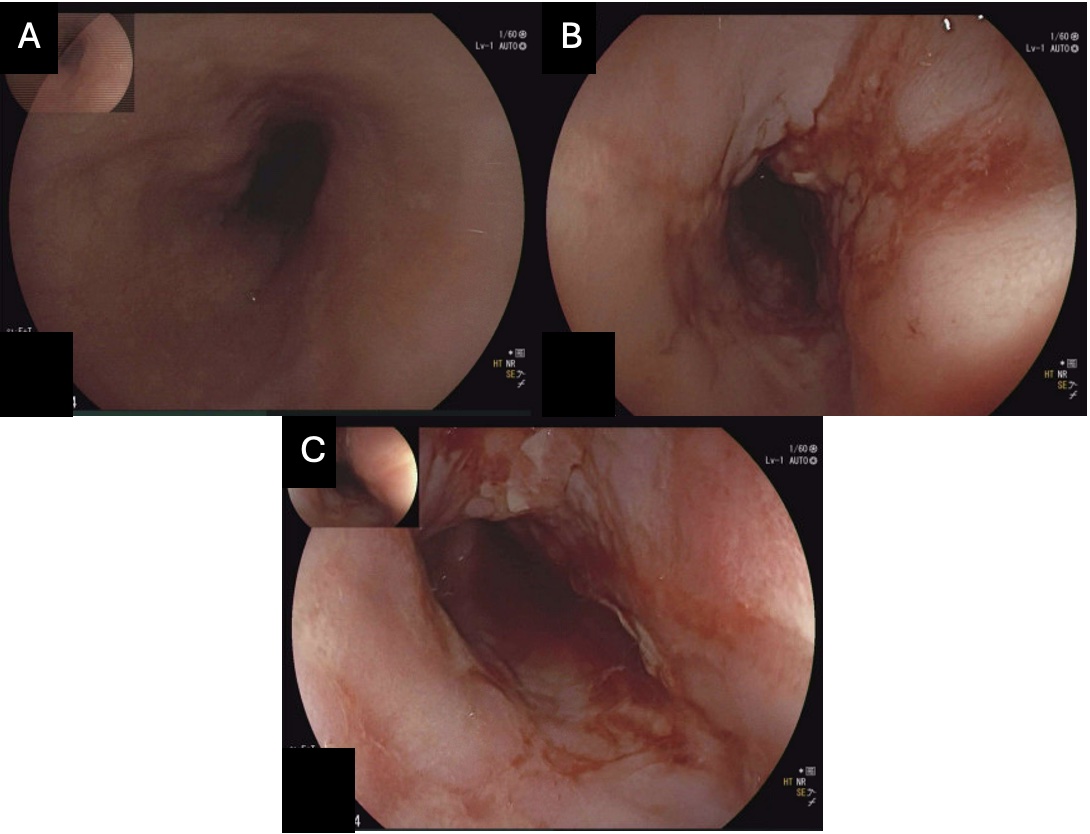
Figure: Figure A. Middle third of the esophagus
Figure B & C. Lower third of esophagus & gastroesophageal junction with ulceration, bleeding and friable mucosa
Figure B & C. Lower third of esophagus & gastroesophageal junction with ulceration, bleeding and friable mucosa
Disclosures:
Joshua Freeman indicated no relevant financial relationships.
Andrew Moore indicated no relevant financial relationships.
Joshua Freeman, DO, Andrew Moore, MD. P0601 - CMV Esophagitis Presenting as Severe Anemia in an Asymptomatic, Immunocompetent Individual, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
