Sunday Poster Session
Category: Esophagus
P0602 - Unexpected Melanoma Metastasis Found in the GI Tract
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- HJ
Hasan Jaber, MD
University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Hasan Jaber, MD1, Mahmoud Mahdi, MD1, Nader Al Souky, MD1, William Palko, MD2, Obada Tayyem, MD3
1University of Kansas School of Medicine, Wichita, KS; 2Wesley Medical Center, Wichita, KS; 3Kansas Gastroenterology and Endoscopy, LLC, Wichita, KS
Introduction: Gastrointestinal (GI) melanomas are rare. Most GI melanomas metastasize from oculocutaneous origins .We herein present a case of metastatic melanoma to the esophagus, stomach, and small bowel during an evaluation for dysphagia.
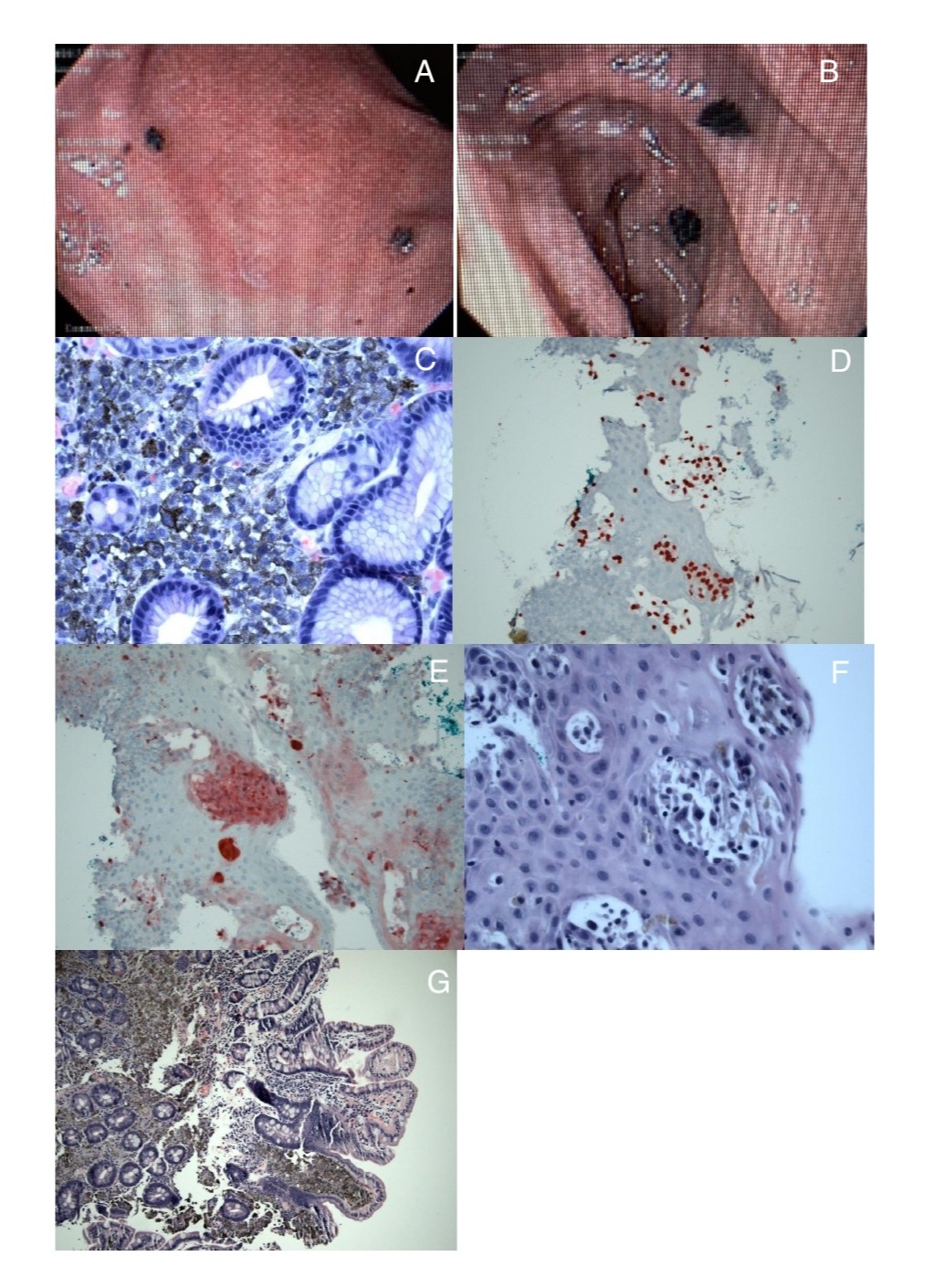
Case Description/Methods: A 62-year-old male presented with weakness, poor oral intake, and unquantified weight loss over several weeks as well as dysphagia, jaundice, and dark urine. Laboratory results showed an INR of 1.2, bilirubin of 6.3 mg/dl, AST of 215 u/l, ALT of 164 u/l, alkaline phosphatase of 554 u/l. A CT scan of the abdomen and pelvis revealed numerous hypoattenuating lesions throughout the liver indicative of metastatic disease. An esophagogastroduodenoscopy (EGD) was performed to evaluate dysphagia, revealing a single hyperpigmented plaque in the upper third of the esophagus as well as hyperpigmented lesions in the stomach and duodenum. Biopsies showed nests of melanocytes with atypical mitosis. Immunohistochemical staining showed positivity for SOX-10, Mart-1, and S100, and negativity for pancytokeratin, supporting the diagnosis of metastatic melanoma. A full examination for a primary cutaneous melanoma revealed a small black ulcerated lesion on the patient's back, which was identified as the primary melanotic lesion. The patient opted for hospice care.
Discussion: The gastrointestinal tract is the second most common site for melanoma metastasis, after the lungs. GI metastases often affect the liver, small intestine, colon, stomach, and esophagus in a descending order of frequency. About 2% of melanomas have an unclear primary source possibly due to the regression of an unknown primary lesion. Depending on their location and size, metastases to the esophagus, stomach, and small bowel can cause symptoms such as dysphagia, abdominal pain, distention, bleeding, obstruction, and intussusception. Endoscopic examination typically reveals distinct lesions, with confirmation through biopsies. Diagnosing GI melanoma needs thorough pathologic examination and immunohistochemical (IHC) testing for markers like S-100, HMB-45, Melan-A, tyrosinase, and neuron-specific enolase. Metastatic melanoma in the GI tract indicates advanced disease, suggesting a poor prognosis. In conclusion, we highlight a rare instance of metastasis to the esophagus, stomach, and small bowel from a primary cutaneous melanoma. When melanoma is incidentally discovered in the GI tract, it is crucial to conduct a thorough assessment, as the patient may have an undiagnosed primary lesion.
Disclosures:
Hasan Jaber, MD1, Mahmoud Mahdi, MD1, Nader Al Souky, MD1, William Palko, MD2, Obada Tayyem, MD3. P0602 - Unexpected Melanoma Metastasis Found in the GI Tract, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Kansas School of Medicine, Wichita, KS; 2Wesley Medical Center, Wichita, KS; 3Kansas Gastroenterology and Endoscopy, LLC, Wichita, KS
Introduction: Gastrointestinal (GI) melanomas are rare. Most GI melanomas metastasize from oculocutaneous origins .We herein present a case of metastatic melanoma to the esophagus, stomach, and small bowel during an evaluation for dysphagia.
Case Description/Methods: A 62-year-old male presented with weakness, poor oral intake, and unquantified weight loss over several weeks as well as dysphagia, jaundice, and dark urine. Laboratory results showed an INR of 1.2, bilirubin of 6.3 mg/dl, AST of 215 u/l, ALT of 164 u/l, alkaline phosphatase of 554 u/l. A CT scan of the abdomen and pelvis revealed numerous hypoattenuating lesions throughout the liver indicative of metastatic disease. An esophagogastroduodenoscopy (EGD) was performed to evaluate dysphagia, revealing a single hyperpigmented plaque in the upper third of the esophagus as well as hyperpigmented lesions in the stomach and duodenum. Biopsies showed nests of melanocytes with atypical mitosis. Immunohistochemical staining showed positivity for SOX-10, Mart-1, and S100, and negativity for pancytokeratin, supporting the diagnosis of metastatic melanoma. A full examination for a primary cutaneous melanoma revealed a small black ulcerated lesion on the patient's back, which was identified as the primary melanotic lesion. The patient opted for hospice care.
Discussion: The gastrointestinal tract is the second most common site for melanoma metastasis, after the lungs. GI metastases often affect the liver, small intestine, colon, stomach, and esophagus in a descending order of frequency. About 2% of melanomas have an unclear primary source possibly due to the regression of an unknown primary lesion. Depending on their location and size, metastases to the esophagus, stomach, and small bowel can cause symptoms such as dysphagia, abdominal pain, distention, bleeding, obstruction, and intussusception. Endoscopic examination typically reveals distinct lesions, with confirmation through biopsies. Diagnosing GI melanoma needs thorough pathologic examination and immunohistochemical (IHC) testing for markers like S-100, HMB-45, Melan-A, tyrosinase, and neuron-specific enolase. Metastatic melanoma in the GI tract indicates advanced disease, suggesting a poor prognosis. In conclusion, we highlight a rare instance of metastasis to the esophagus, stomach, and small bowel from a primary cutaneous melanoma. When melanoma is incidentally discovered in the GI tract, it is crucial to conduct a thorough assessment, as the patient may have an undiagnosed primary lesion.
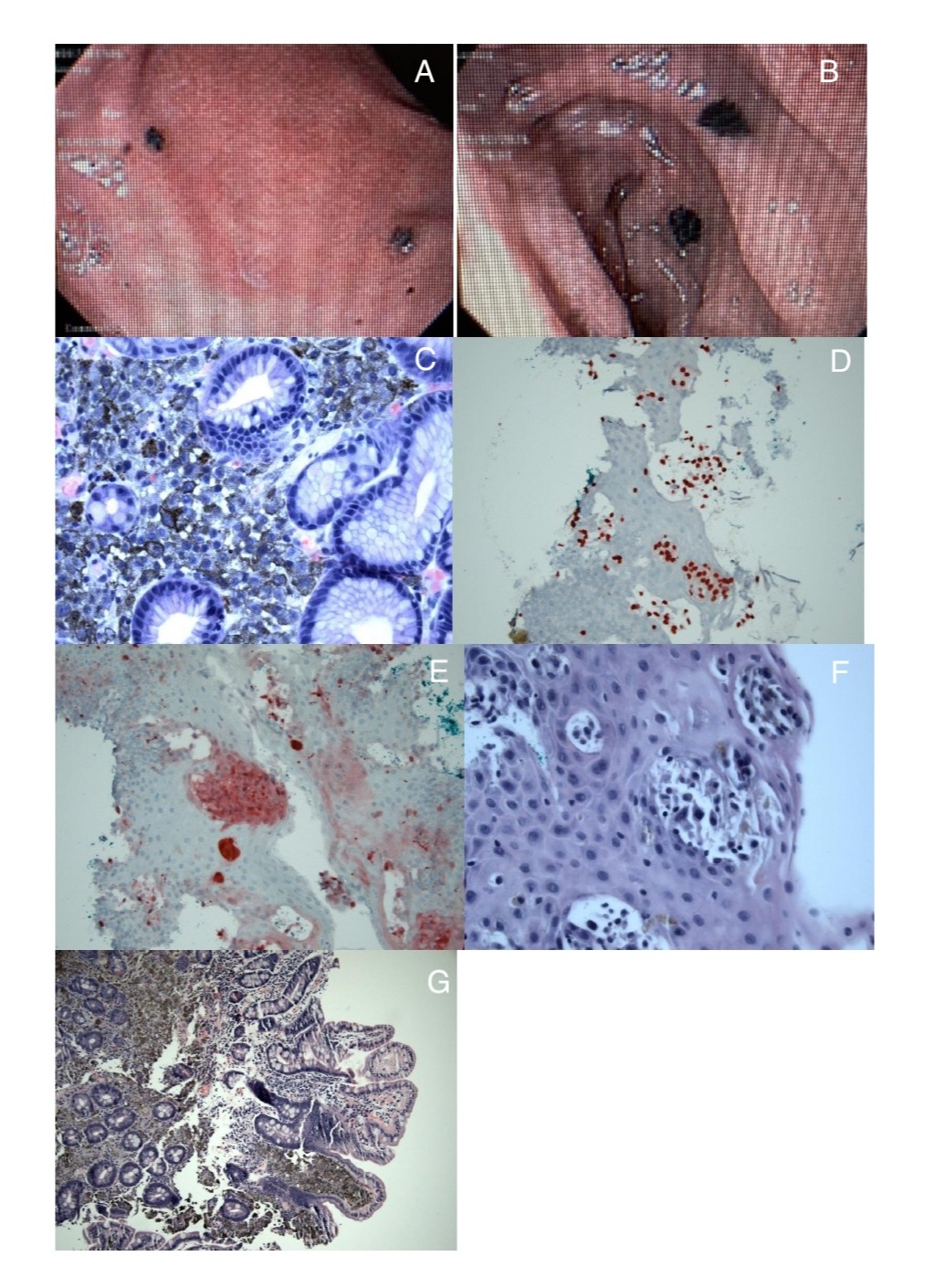
Figure: Figure 1: (A) Melanoma deposits in stomach (B) Melanoma deposits in small bowel (C) Melanoma deposits in stomach under 40x magnification (D) Melanoma deposits in esophagus with SOX10 stain (E) Melanoma deposits in esophagus with S100 stain (F) Melanoma deposits in esophagus under 40x magnification (G) Melanoma deposits in duodenum under 10x magnification
Disclosures:
Hasan Jaber indicated no relevant financial relationships.
Mahmoud Mahdi indicated no relevant financial relationships.
Nader Al Souky indicated no relevant financial relationships.
William Palko indicated no relevant financial relationships.
Obada Tayyem indicated no relevant financial relationships.
Hasan Jaber, MD1, Mahmoud Mahdi, MD1, Nader Al Souky, MD1, William Palko, MD2, Obada Tayyem, MD3. P0602 - Unexpected Melanoma Metastasis Found in the GI Tract, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
