Sunday Poster Session
Category: Functional Bowel Disease
P0628 - Abdominal Pain in Gastroparesis: Comparing PAGI-SYM and SF-8 Survey Scores Among Opiate and Non-Opiate Analgesic Management
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

John Ebeid, MD
Temple University Hospital
Philadelphia, PA
Presenting Author(s)
Abraham Ifrah, MD1, Henry P. Parkman, MD2, John Ebeid, MD1
1Temple University Hospital, Philadelphia, PA; 2Temple University, Strafford, PA
Introduction: Abdominal pain (AP) is a difficult symptom to treat in patients with gastroparesis (GP). Despite evidence that opiate analgesics worsen GP, providers prescribe them when other options fail. Some patients with GP use opiates for abdominal pain but also for non-AP syndromes. This study evaluates how patients with GP manage AP, and if differences exist in rating AP severity between patients who use opiate analgesics for AP and those who use opiate analgesics for non-AP symptoms.
Methods: Patients at a tertiary academic center gastroenterology clinic completed Patient Assessment of Upper Gastrointestinal Disorders Symptoms Questionnaire and QOL-SF8 surveys. Patients recorded GP treatments, pain treatments and indication, and any hospitalizations/Emergency Department visits within 3 months of clinic visit.
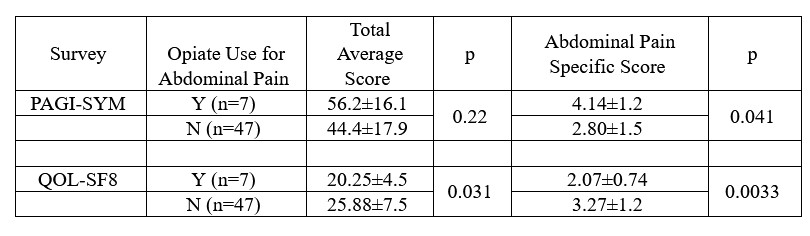
Results: 54 patients completed the survey. 72% reported AP, 98% reporting that AP was part of GP symptoms. Mean body mass index was 26.8 and mean age was 45 years. Patients reported managing AP with 31.3% using nothing, 25% ice, hot showers or heating pads, 20.8% acetaminophen, 14.6% hyoscyamine, 11% opiate analgesics, 11% marijuana, 8.3% NSAIDs, 3.7% benzodiazepines, 2.1% calcium carbonate, 2.1% dicyclomine, 2.1% domperidone, and 2.1% gabapentin. The reasons for using opiates were: 58% AP, 8.3% arthritis, with all patients reporting daily use. Average PAGI-SYM AP severity scores were higher in patients using opiates for AP than non-AP (4.14±1.2 v 2.80±1.5, p=0.041). Patients taking opiates for AP had more morphine milliequivalent use than for non-AP (77.5±21.9 vs. 31.8±14.1; p=0.037). Patients using opiates for AP had more emergency room visits than non-AP. QOL-SF8 scores were lower for patients reporting use of opiates vs. patients not reporting opiate use (20.25±4.5 vs. 25.88±7.5, p=0.031). QOL-SF8 pain specific scores were lower for patients taking opiates for AP compared to those taking for non-AP (2.07±0.74 vs. 3.27±1.2; p=0.0033).
Discussion: In this study, 72% of patients surveyed reported AP. 13% of patients were taking opiates. Patients using opiate analgesics had lower overall QOL-SF8 scores, indicating poorer quality of life. Patients who used opiate analgesics for AP had greater average AP severity score and used more opiates than patients using opiates for musculoskeletal pain. This data suggests that patients using opiates may have an additional mechanism contributing to AP compared to patients using opiates for non-AP.
Disclosures:
Abraham Ifrah, MD1, Henry P. Parkman, MD2, John Ebeid, MD1. P0628 - Abdominal Pain in Gastroparesis: Comparing PAGI-SYM and SF-8 Survey Scores Among Opiate and Non-Opiate Analgesic Management, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Temple University Hospital, Philadelphia, PA; 2Temple University, Strafford, PA
Introduction: Abdominal pain (AP) is a difficult symptom to treat in patients with gastroparesis (GP). Despite evidence that opiate analgesics worsen GP, providers prescribe them when other options fail. Some patients with GP use opiates for abdominal pain but also for non-AP syndromes. This study evaluates how patients with GP manage AP, and if differences exist in rating AP severity between patients who use opiate analgesics for AP and those who use opiate analgesics for non-AP symptoms.
Methods: Patients at a tertiary academic center gastroenterology clinic completed Patient Assessment of Upper Gastrointestinal Disorders Symptoms Questionnaire and QOL-SF8 surveys. Patients recorded GP treatments, pain treatments and indication, and any hospitalizations/Emergency Department visits within 3 months of clinic visit.
Results: 54 patients completed the survey. 72% reported AP, 98% reporting that AP was part of GP symptoms. Mean body mass index was 26.8 and mean age was 45 years. Patients reported managing AP with 31.3% using nothing, 25% ice, hot showers or heating pads, 20.8% acetaminophen, 14.6% hyoscyamine, 11% opiate analgesics, 11% marijuana, 8.3% NSAIDs, 3.7% benzodiazepines, 2.1% calcium carbonate, 2.1% dicyclomine, 2.1% domperidone, and 2.1% gabapentin. The reasons for using opiates were: 58% AP, 8.3% arthritis, with all patients reporting daily use. Average PAGI-SYM AP severity scores were higher in patients using opiates for AP than non-AP (4.14±1.2 v 2.80±1.5, p=0.041). Patients taking opiates for AP had more morphine milliequivalent use than for non-AP (77.5±21.9 vs. 31.8±14.1; p=0.037). Patients using opiates for AP had more emergency room visits than non-AP. QOL-SF8 scores were lower for patients reporting use of opiates vs. patients not reporting opiate use (20.25±4.5 vs. 25.88±7.5, p=0.031). QOL-SF8 pain specific scores were lower for patients taking opiates for AP compared to those taking for non-AP (2.07±0.74 vs. 3.27±1.2; p=0.0033).
Discussion: In this study, 72% of patients surveyed reported AP. 13% of patients were taking opiates. Patients using opiate analgesics had lower overall QOL-SF8 scores, indicating poorer quality of life. Patients who used opiate analgesics for AP had greater average AP severity score and used more opiates than patients using opiates for musculoskeletal pain. This data suggests that patients using opiates may have an additional mechanism contributing to AP compared to patients using opiates for non-AP.
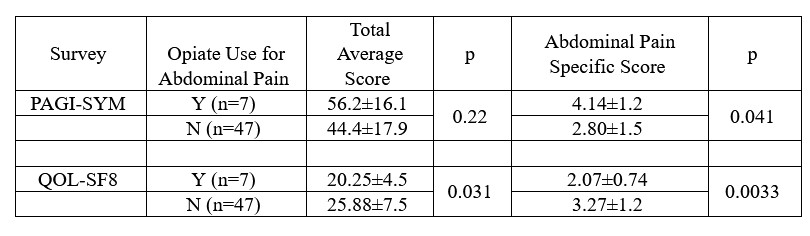
Figure: Table 1. Comparison via PAGI-SYM, QOL-SF8 of patients using and those not using opiates for abdominal pain.
Disclosures:
Abraham Ifrah indicated no relevant financial relationships.
Henry Parkman: Evoke Pharma – Consultant. Medtronic Enterra – Consultant. Takeda – Consultant.
John Ebeid indicated no relevant financial relationships.
Abraham Ifrah, MD1, Henry P. Parkman, MD2, John Ebeid, MD1. P0628 - Abdominal Pain in Gastroparesis: Comparing PAGI-SYM and SF-8 Survey Scores Among Opiate and Non-Opiate Analgesic Management, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
