Sunday Poster Session
Category: Functional Bowel Disease
P0640 - Resilience in Patients With Functional Dyspepsia: A Prospective Questionnaire Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- BL
Brian E. Lacy, MD, PhD, FACG
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Robert C. Chase, MD1, David J. Cangemi, MD1, Laurie Keefer, PhD2, Katherine J. Chase, MSc1, Brian E. Lacy, MD, PhD, FACG1
1Mayo Clinic, Jacksonville, FL; 2Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Functional Dyspepsia (FD), a common disorder of gut-brain interaction, is associated with alterations in gastric accommodation, gastric emptying, gastric sensitivity, gastroduodenal permeability, and the gut microbiome. Resilience, the ability to maintain function under personal or physical stress, may play a role in development of FD, although no studies have evaluated this theory. We hypothesize that FD patients have lower resilience than the general population, which may lead to a new therapeutic target.
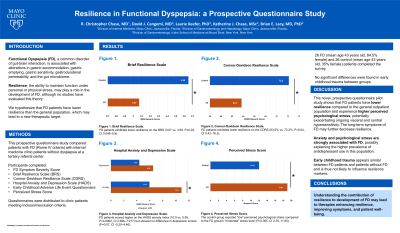
Methods: This prospective questionnaire study compared patients with FD (Rome IV criteria) with internal medicine clinic patients without dyspepsia at a tertiary referral center. Participants completed the FD symptom severity score [2], Brief Resilience Scale (BRS) [3], Connor-Davidson Resilience Scale (CDRS) [4], hospital anxiety and depression scale (HADS) [5,6], early childhood adverse life event questionnaire [7], and perceived stress score [8]. Questionnaires were distributed to clinic patients meeting inclusion/exclusion criteria.
Results: 26 FD (mean age 43 years old, 84.5% female) and 26 control (mean age 43 years old, 35% female) patients completed the survey. FD patients exhibited lower resilience on the BRS (3.07 vs. 3.65, P=0.03, CI 0.046–0.9) and CDRS (63.5% vs. 72.2%, P=0.04, CI 0.42–16.5). FD patients scored higher on the HADS anxiety index (10.9 vs. 5.95, P=0.0002, CI 2.696–7.217) but showed no difference in depression scores (P=0.07, CI -0.20–4.46). The control group reported "low" perceived psychological stress compared to the FD group's "moderate" stress level (P=0.005, CI 2.35–11.65). No significant differences were found in early childhood trauma between groups.
Discussion: This novel, prospective questionnaire pilot study shows that FD patients have lower resilience compared to the general outpatient population and experience higher perceived psychological stress, potentially exacerbating ongoing visceral and central hypersensitivity. The long-term symptoms of FD may further decrease resilience. Anxiety and psychological stress are strongly associated with FD, possibly explaining the higher prevalence of antidepressant use in this population [9]. Early childhood trauma appears similar between FD patients and patients without FD and is thus not likely to influence resilience markers [10]. Understanding the contribution of resilience to development of FD may lead to therapies enhancing resilience, improving symptoms, and patient well-being.
Disclosures:
Robert C. Chase, MD1, David J. Cangemi, MD1, Laurie Keefer, PhD2, Katherine J. Chase, MSc1, Brian E. Lacy, MD, PhD, FACG1. P0640 - Resilience in Patients With Functional Dyspepsia: A Prospective Questionnaire Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic, Jacksonville, FL; 2Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Functional Dyspepsia (FD), a common disorder of gut-brain interaction, is associated with alterations in gastric accommodation, gastric emptying, gastric sensitivity, gastroduodenal permeability, and the gut microbiome. Resilience, the ability to maintain function under personal or physical stress, may play a role in development of FD, although no studies have evaluated this theory. We hypothesize that FD patients have lower resilience than the general population, which may lead to a new therapeutic target.
Methods: This prospective questionnaire study compared patients with FD (Rome IV criteria) with internal medicine clinic patients without dyspepsia at a tertiary referral center. Participants completed the FD symptom severity score [2], Brief Resilience Scale (BRS) [3], Connor-Davidson Resilience Scale (CDRS) [4], hospital anxiety and depression scale (HADS) [5,6], early childhood adverse life event questionnaire [7], and perceived stress score [8]. Questionnaires were distributed to clinic patients meeting inclusion/exclusion criteria.
Results: 26 FD (mean age 43 years old, 84.5% female) and 26 control (mean age 43 years old, 35% female) patients completed the survey. FD patients exhibited lower resilience on the BRS (3.07 vs. 3.65, P=0.03, CI 0.046–0.9) and CDRS (63.5% vs. 72.2%, P=0.04, CI 0.42–16.5). FD patients scored higher on the HADS anxiety index (10.9 vs. 5.95, P=0.0002, CI 2.696–7.217) but showed no difference in depression scores (P=0.07, CI -0.20–4.46). The control group reported "low" perceived psychological stress compared to the FD group's "moderate" stress level (P=0.005, CI 2.35–11.65). No significant differences were found in early childhood trauma between groups.
Discussion: This novel, prospective questionnaire pilot study shows that FD patients have lower resilience compared to the general outpatient population and experience higher perceived psychological stress, potentially exacerbating ongoing visceral and central hypersensitivity. The long-term symptoms of FD may further decrease resilience. Anxiety and psychological stress are strongly associated with FD, possibly explaining the higher prevalence of antidepressant use in this population [9]. Early childhood trauma appears similar between FD patients and patients without FD and is thus not likely to influence resilience markers [10]. Understanding the contribution of resilience to development of FD may lead to therapies enhancing resilience, improving symptoms, and patient well-being.
Disclosures:
Robert Chase indicated no relevant financial relationships.
David Cangemi indicated no relevant financial relationships.
Laurie Keefer: ardelyx – Consultant, Grant/Research Support. coprata health\ – Advisory Committee/Board Member. pfizer – Consultant. trellus health – Consultant, Stock-publicly held company(excluding mutual/index funds).
Katherine Chase indicated no relevant financial relationships.
Brian Lacy: AbbVie – Consultant. Ardelyx – Consultant. Gemelli Biotech – Consultant. Ironwood Pharmaceuticals – Consultant. Salix Pharmaceuticals – Consultant. Takeda – Consultant.
Robert C. Chase, MD1, David J. Cangemi, MD1, Laurie Keefer, PhD2, Katherine J. Chase, MSc1, Brian E. Lacy, MD, PhD, FACG1. P0640 - Resilience in Patients With Functional Dyspepsia: A Prospective Questionnaire Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
