Sunday Poster Session
Category: General Endoscopy
P0685 - Utilization of Gastrointestinal Procedures Before and After Palliative Care Initiation: A TriNetX Database Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Yichen Wang, MD
University of Pennsylvania
Philadelphia, PA
Presenting Author(s)
Yichen Wang, MD1, Yuting Huang, MBBS, PhD2, Chukwunonso Ezeani, MBBS3, Lekhya Kollu, BA4, Philip Okafor, MD, MPH2
1University of Pennsylvania, Philadelphia, PA; 2Mayo Clinic, Jacksonville, FL; 3Baton Rouge General Medical Center, Baton Rouge, LA; 4Lewis Katz School of Medicine at Temple University, Philadelphia, PA
Introduction: Palliative care is integral in improving the quality of life for patients with serious illnesses. This study aims to assess the utilization of gastrointestinal (GI) procedures before and after the first palliative care encounter.
Methods: We utilized the TriNetX database, a global federated research network that provides data across both inpatient and outpatient settings. Patients with palliative care encounters between January 1, 2017, and June 12, 2024, were included. Palliative care encounters were identified using the International Classification of Diseases, Tenth Revision (ICD-10) code Z51.5. GI procedures were identified using ICD-10 procedural coding system codes beginning with "0D", with specific procedures categorized using the corresponding root operation codes. The start date ensures that the analysis encompasses data post-ICD-9 to ICD-10 transition, enhancing study accuracy. Statistical differences in GI procedure rates before and after the first palliative care encounter were analyzed using the one-sample test of proportions.
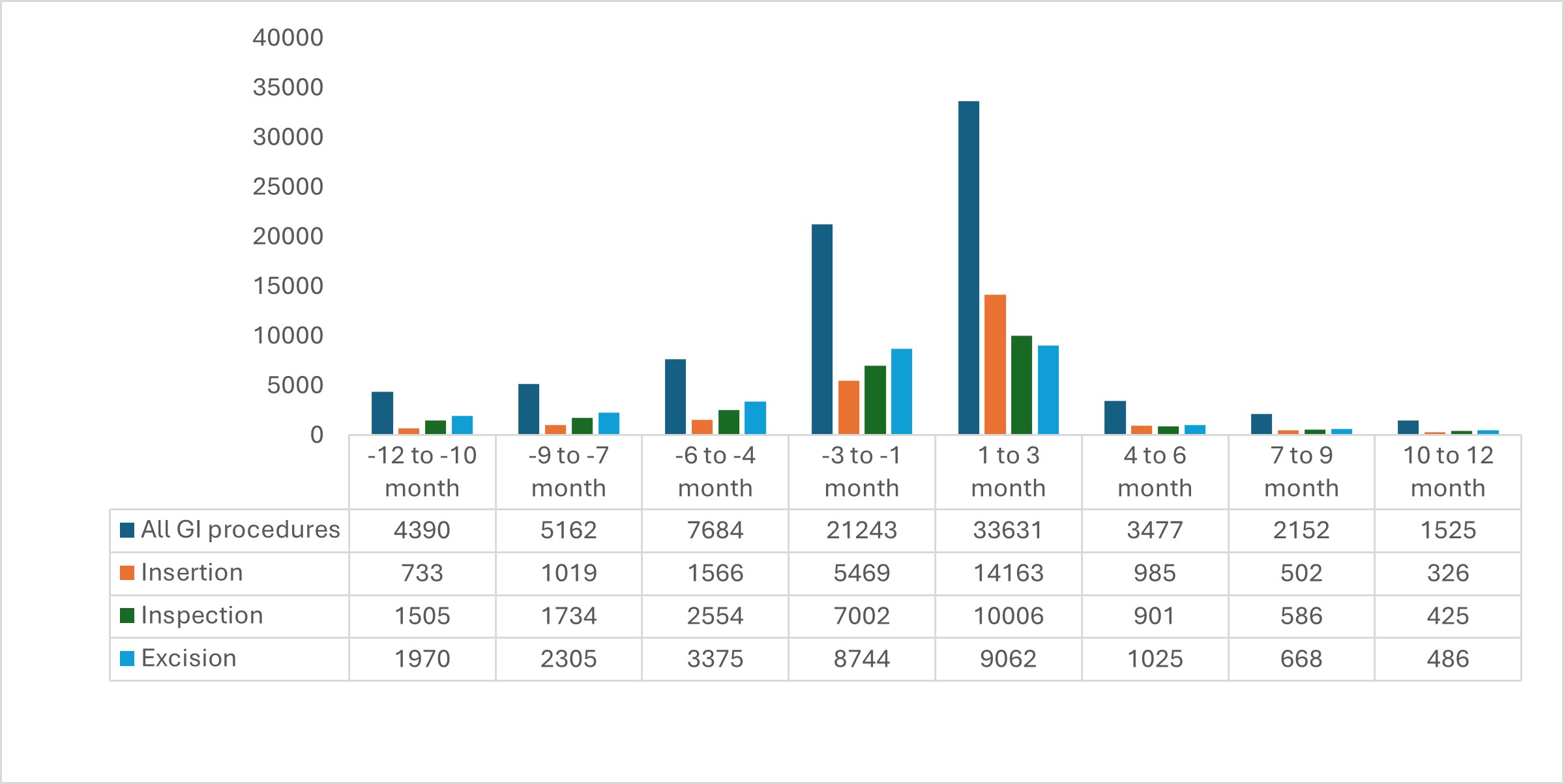
Results: A total of 400,283 patients were included. The mean age at the first palliative care encounter was 69.8 years; 46.9% were female. Characteristics of patients at palliative care encounters can be found in Table 1. Within one year before the first palliative care encounter, 33,139 (8.3%) patients underwent GI procedures, including 2.0% for device insertion (e.g., stent and feeding tube placement), 2.9% for inspection (e.g., endoscopic examination), and 3.8% for excision (e.g., biopsy or partial resection). One year after the first palliative care encounter, 41,349 (10.3%) patients had GI procedures, categorized as 4.1% for insertion, 3.1% for inspection, and 3.0% for excision, indicating a significant increase post-palliative encounter (P < 0.001). When limited to three months before and after the first palliative care encounter, 21,243 (5.1%) and 33,631 (8.2%) patients underwent GI procedures, respectively (Figure 1).
Discussion: Choosing between interventional palliation and comfort care in the final stages of life is equally challenging and requires immense courage. Our study reveals a significant increase in GI procedures after initiating palliative care, especially in the early phase, highlighting a high demand for these interventions. This underscores the need for patients, families, and clinicians to engage in thoughtful dialogue, ensuring decisions align with the patient’s values and wishes, ultimately honoring the end-of-life journey.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Yichen Wang, MD1, Yuting Huang, MBBS, PhD2, Chukwunonso Ezeani, MBBS3, Lekhya Kollu, BA4, Philip Okafor, MD, MPH2. P0685 - Utilization of Gastrointestinal Procedures Before and After Palliative Care Initiation: A TriNetX Database Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Pennsylvania, Philadelphia, PA; 2Mayo Clinic, Jacksonville, FL; 3Baton Rouge General Medical Center, Baton Rouge, LA; 4Lewis Katz School of Medicine at Temple University, Philadelphia, PA
Introduction: Palliative care is integral in improving the quality of life for patients with serious illnesses. This study aims to assess the utilization of gastrointestinal (GI) procedures before and after the first palliative care encounter.
Methods: We utilized the TriNetX database, a global federated research network that provides data across both inpatient and outpatient settings. Patients with palliative care encounters between January 1, 2017, and June 12, 2024, were included. Palliative care encounters were identified using the International Classification of Diseases, Tenth Revision (ICD-10) code Z51.5. GI procedures were identified using ICD-10 procedural coding system codes beginning with "0D", with specific procedures categorized using the corresponding root operation codes. The start date ensures that the analysis encompasses data post-ICD-9 to ICD-10 transition, enhancing study accuracy. Statistical differences in GI procedure rates before and after the first palliative care encounter were analyzed using the one-sample test of proportions.
Results: A total of 400,283 patients were included. The mean age at the first palliative care encounter was 69.8 years; 46.9% were female. Characteristics of patients at palliative care encounters can be found in Table 1. Within one year before the first palliative care encounter, 33,139 (8.3%) patients underwent GI procedures, including 2.0% for device insertion (e.g., stent and feeding tube placement), 2.9% for inspection (e.g., endoscopic examination), and 3.8% for excision (e.g., biopsy or partial resection). One year after the first palliative care encounter, 41,349 (10.3%) patients had GI procedures, categorized as 4.1% for insertion, 3.1% for inspection, and 3.0% for excision, indicating a significant increase post-palliative encounter (P < 0.001). When limited to three months before and after the first palliative care encounter, 21,243 (5.1%) and 33,631 (8.2%) patients underwent GI procedures, respectively (Figure 1).
Discussion: Choosing between interventional palliation and comfort care in the final stages of life is equally challenging and requires immense courage. Our study reveals a significant increase in GI procedures after initiating palliative care, especially in the early phase, highlighting a high demand for these interventions. This underscores the need for patients, families, and clinicians to engage in thoughtful dialogue, ensuring decisions align with the patient’s values and wishes, ultimately honoring the end-of-life journey.
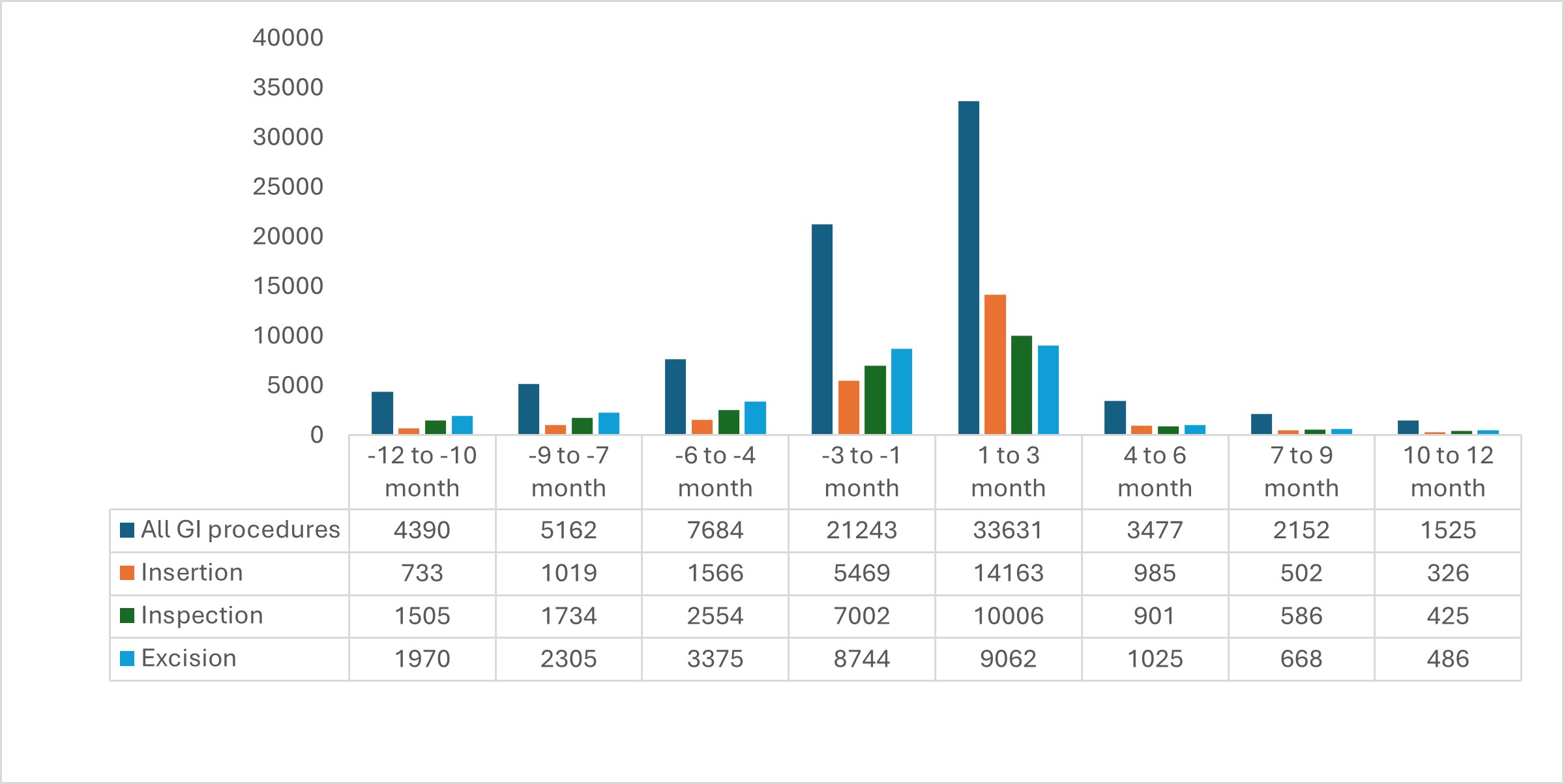
Figure: Figure 1. Utilization of Gastrointestinal Procedures Before and After Initial Palliative Care Encounter
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Yichen Wang indicated no relevant financial relationships.
Yuting Huang indicated no relevant financial relationships.
Chukwunonso Ezeani indicated no relevant financial relationships.
Lekhya Kollu indicated no relevant financial relationships.
Philip Okafor indicated no relevant financial relationships.
Yichen Wang, MD1, Yuting Huang, MBBS, PhD2, Chukwunonso Ezeani, MBBS3, Lekhya Kollu, BA4, Philip Okafor, MD, MPH2. P0685 - Utilization of Gastrointestinal Procedures Before and After Palliative Care Initiation: A TriNetX Database Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
