Sunday Poster Session
Category: General Endoscopy
P0697 - Percutaneous Gastrostomy Tube Placement in a Patient With Rectus Sheath Hematoma: A Case Report and Discussion
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- WH
William R. Henry, MD
University of Mississippi Medical Center
Jackson, MS
Presenting Author(s)
William R. Henry, MD, Kaitlyn Cronk, MD, Ismail Ganim, MD, Shou-jiang Tang, MD
University of Mississippi Medical Center, Jackson, MS
Introduction: Rectus sheath hematoma (RSH) is a relatively rare condition resulting from bleeding into the rectus sheath after damage to the epigastric arteries or by direct muscular tear. RSH has been strongly associated with abdominal trauma and anticoagulation. It typically presents with abdominal pain, palpable abdominal wall mass, tenderness and guarding. RSH is generally considered to be a self-limiting condition that can be treated conservatively, but it may also be fatal in some cases.
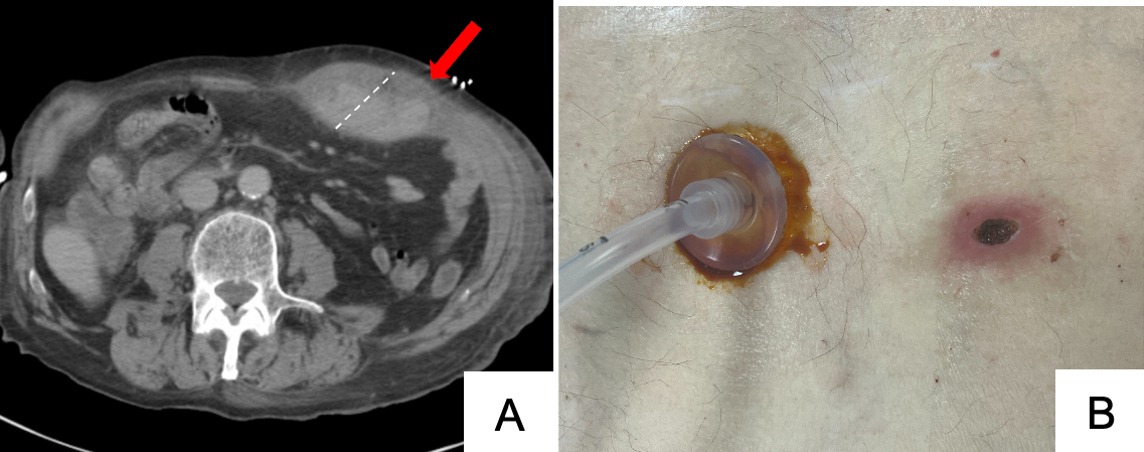
Case Description/Methods: We present a case of an 84-year-old male with history of atrial fibrillation on anticoagulation who presented after a motor vehicle collision with acute metabolic encephalopathy secondary to acute cystitis. During hospitalization, he was deemed unsafe for intake by mouth and an alternative source of nutrition was recommended. A percutaneous gastrostomy tube (PGT) was placed endoscopically; however, the patient pulled out the PGT and developed a RSH. After a multidisciplinary discussion with Surgery and Radiology, it was thought that a second feeding tube could not be placed until full resolution of the hematoma. However, this hindered the patient from discharging to a long-term facility. After discussing the risks and benefits of the procedure with family and repeat scans noted the hematoma was confined lateral to the linea alba, the decision was made to proceed with PGT placement. Careful consideration was taken during the procedure. Confirmation of the site before trochanter placement was obtained using 1:1 motion, transillumination, and visualization of the local anesthetic needle. The procedure was successful, and the patient tolerated enteral feeding well without any post-procedure complications.
Discussion: The management of PGT placement in patients with RSH include risks of infection, hemorrhage, and hematoma expansion that must be carefully weighed against the benefits of the procedure. Confirmatory modalities such as 1:1 motion with direct endoscopic visualization, transillumination, and visualization of the anesthetic needle tip before trochanter placement can be valuable in guiding PGT placement and minimizing risks of complications. Close monitoring for expansion of the hematoma and bleeding post-procedure is essential. Further research is critical to establish guidelines for endoscopic PGT placement in patients with RSH to optimize patient outcomes and minimize associated complications.
Disclosures:
William R. Henry, MD, Kaitlyn Cronk, MD, Ismail Ganim, MD, Shou-jiang Tang, MD. P0697 - Percutaneous Gastrostomy Tube Placement in a Patient With Rectus Sheath Hematoma: A Case Report and Discussion, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Mississippi Medical Center, Jackson, MS
Introduction: Rectus sheath hematoma (RSH) is a relatively rare condition resulting from bleeding into the rectus sheath after damage to the epigastric arteries or by direct muscular tear. RSH has been strongly associated with abdominal trauma and anticoagulation. It typically presents with abdominal pain, palpable abdominal wall mass, tenderness and guarding. RSH is generally considered to be a self-limiting condition that can be treated conservatively, but it may also be fatal in some cases.
Case Description/Methods: We present a case of an 84-year-old male with history of atrial fibrillation on anticoagulation who presented after a motor vehicle collision with acute metabolic encephalopathy secondary to acute cystitis. During hospitalization, he was deemed unsafe for intake by mouth and an alternative source of nutrition was recommended. A percutaneous gastrostomy tube (PGT) was placed endoscopically; however, the patient pulled out the PGT and developed a RSH. After a multidisciplinary discussion with Surgery and Radiology, it was thought that a second feeding tube could not be placed until full resolution of the hematoma. However, this hindered the patient from discharging to a long-term facility. After discussing the risks and benefits of the procedure with family and repeat scans noted the hematoma was confined lateral to the linea alba, the decision was made to proceed with PGT placement. Careful consideration was taken during the procedure. Confirmation of the site before trochanter placement was obtained using 1:1 motion, transillumination, and visualization of the local anesthetic needle. The procedure was successful, and the patient tolerated enteral feeding well without any post-procedure complications.
Discussion: The management of PGT placement in patients with RSH include risks of infection, hemorrhage, and hematoma expansion that must be carefully weighed against the benefits of the procedure. Confirmatory modalities such as 1:1 motion with direct endoscopic visualization, transillumination, and visualization of the anesthetic needle tip before trochanter placement can be valuable in guiding PGT placement and minimizing risks of complications. Close monitoring for expansion of the hematoma and bleeding post-procedure is essential. Further research is critical to establish guidelines for endoscopic PGT placement in patients with RSH to optimize patient outcomes and minimize associated complications.
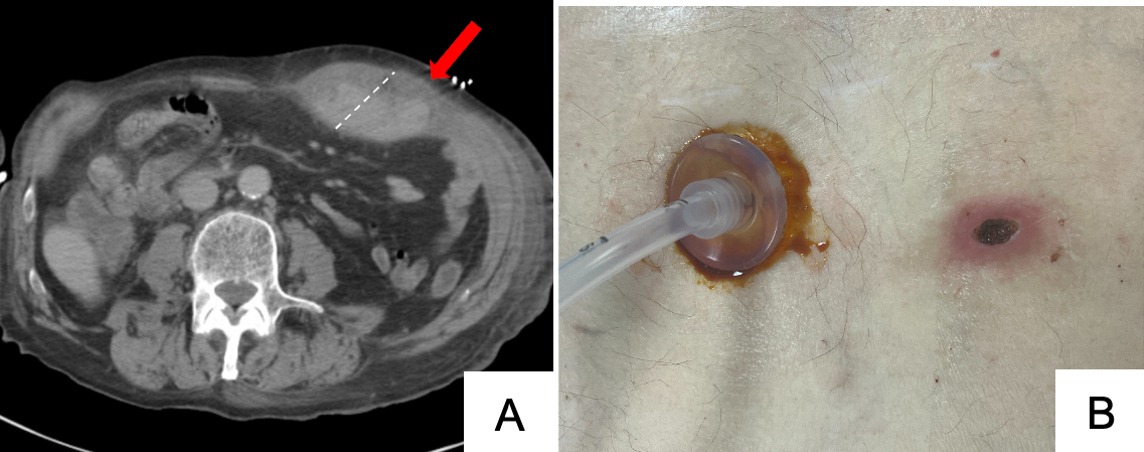
Figure: A. Rectus sheath hematoma on axial CT. B. Successful placement of PEG tube.
Disclosures:
William Henry indicated no relevant financial relationships.
Kaitlyn Cronk indicated no relevant financial relationships.
Ismail Ganim indicated no relevant financial relationships.
Shou-jiang Tang indicated no relevant financial relationships.
William R. Henry, MD, Kaitlyn Cronk, MD, Ismail Ganim, MD, Shou-jiang Tang, MD. P0697 - Percutaneous Gastrostomy Tube Placement in a Patient With Rectus Sheath Hematoma: A Case Report and Discussion, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
