Sunday Poster Session
Category: General Endoscopy
P0708 - A Rare Case of Gastric Perforation During the PEG Tube Placement in a Severe Malnutrition Patient
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
- YY
Yan Yan, MBBS, PhD
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Yan Yan, MBBS, PhD, Rex Siu, MD, Yan Bi, MD, PhD, Victoria Gómez, MD, Vivek Kumbhari, MBChB, PhD, Yuting Huang, MBBS, PhD
Mayo Clinic, Jacksonville, FL
Introduction: PEG and PEG-J tubes are frequently used for patients unable to tolerate oral nutrition and requiring long-term nutritional support. Despite a high success rate, complications such as hemorrhage, aspiration pneumonia, buried bumper syndrome, necrotizing fasciitis, bowel perforation, and metastatic seeding have been reported.
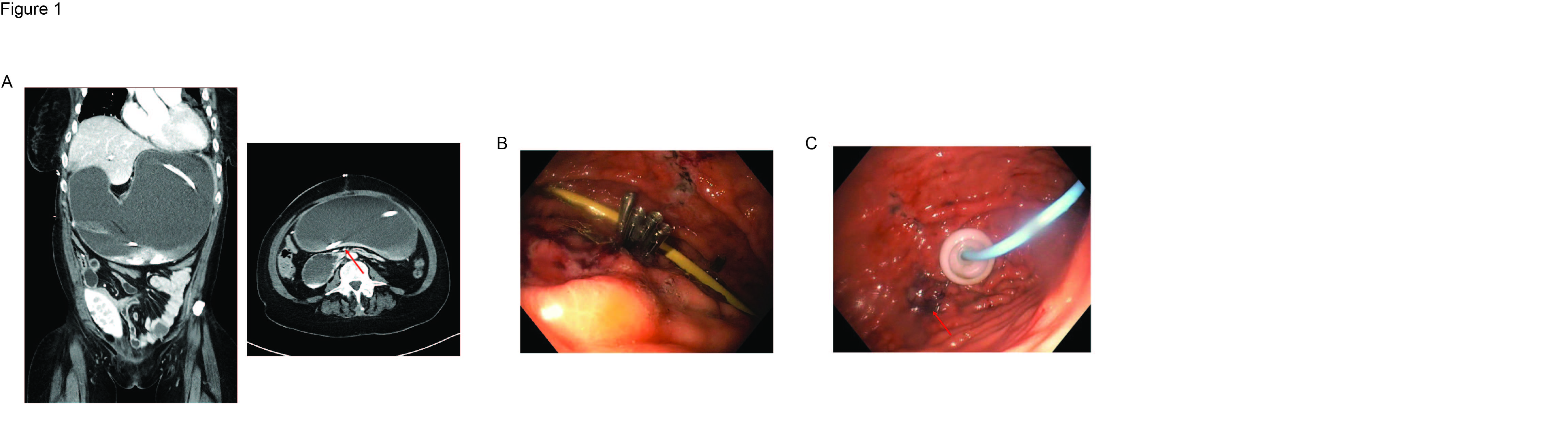
Case Description/Methods: A 43-year-old female patient with severe malnutrition in the ICU was consulted for PEG-J tube placement due to superior mesenteric artery (SMA) syndrome. Her medical history includes hypertension, hyperlipidemia, end-stage renal disease (ESRD), systemic lupus erythematosus (SLE), interstitial lung disease (ILD), and pulmonary hypertension. She also had lung and kidney transplants; hemicolectomy one month before consultation. Contrast CT scan indicated massive dilation of the esophagus, stomach, and proximal duodenum (Figure 1A). EGD revealed a normal esophagus but moderate inflammation throughout the stomach, and a dilated duodenum. Following evaluation, the patient underwent the placement of a PEG. After placement, a gastric perforation was found during the post-PEG evaluation with the gastroscope, evidence by the inner bumper found in the peritoneum. To manage the perforation, immediate aspiration of gastric contents was performed, and the perforation site was temporarily closed with four clips (Figure 1B). The following day, the second EDG was performed, revealing a 5 mm anterior gastric wall defect, which was closed with a clip. PEG was then inserted adjacent to the clip, and endoscopy confirmed a proper placement (Figure 1C). Patient received tube feeding for 11 months. PEG tube was removed when the oral intake meets nutrition requirements. No GI symptoms were reported at the time of follow up.
Discussion: Gastric perforation during PEG placement is rare. In our case, we believe contributors included severe malnutrition and pre-existing gastric mucosal damage associated with recent transplant surgery, and multiple chronic diseases. In setting of perforation, timely aspirate of gastric content, and surgery consult are essential. For full thickness defects in the stomach, OTSC is preferred than TTS. The OTSC allows for full thickness closure and is so robust that we are confident to proceed with rapidly expanding the stomach to place a new PEG. In summary, this case highlights the possibility of gastric perforation in severe malnutrition patients, suggesting timely diagnosis and management of perforation are critical to improve patient outcomes.
Disclosures:
Yan Yan, MBBS, PhD, Rex Siu, MD, Yan Bi, MD, PhD, Victoria Gómez, MD, Vivek Kumbhari, MBChB, PhD, Yuting Huang, MBBS, PhD. P0708 - A Rare Case of Gastric Perforation During the PEG Tube Placement in a Severe Malnutrition Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mayo Clinic, Jacksonville, FL
Introduction: PEG and PEG-J tubes are frequently used for patients unable to tolerate oral nutrition and requiring long-term nutritional support. Despite a high success rate, complications such as hemorrhage, aspiration pneumonia, buried bumper syndrome, necrotizing fasciitis, bowel perforation, and metastatic seeding have been reported.
Case Description/Methods: A 43-year-old female patient with severe malnutrition in the ICU was consulted for PEG-J tube placement due to superior mesenteric artery (SMA) syndrome. Her medical history includes hypertension, hyperlipidemia, end-stage renal disease (ESRD), systemic lupus erythematosus (SLE), interstitial lung disease (ILD), and pulmonary hypertension. She also had lung and kidney transplants; hemicolectomy one month before consultation. Contrast CT scan indicated massive dilation of the esophagus, stomach, and proximal duodenum (Figure 1A). EGD revealed a normal esophagus but moderate inflammation throughout the stomach, and a dilated duodenum. Following evaluation, the patient underwent the placement of a PEG. After placement, a gastric perforation was found during the post-PEG evaluation with the gastroscope, evidence by the inner bumper found in the peritoneum. To manage the perforation, immediate aspiration of gastric contents was performed, and the perforation site was temporarily closed with four clips (Figure 1B). The following day, the second EDG was performed, revealing a 5 mm anterior gastric wall defect, which was closed with a clip. PEG was then inserted adjacent to the clip, and endoscopy confirmed a proper placement (Figure 1C). Patient received tube feeding for 11 months. PEG tube was removed when the oral intake meets nutrition requirements. No GI symptoms were reported at the time of follow up.
Discussion: Gastric perforation during PEG placement is rare. In our case, we believe contributors included severe malnutrition and pre-existing gastric mucosal damage associated with recent transplant surgery, and multiple chronic diseases. In setting of perforation, timely aspirate of gastric content, and surgery consult are essential. For full thickness defects in the stomach, OTSC is preferred than TTS. The OTSC allows for full thickness closure and is so robust that we are confident to proceed with rapidly expanding the stomach to place a new PEG. In summary, this case highlights the possibility of gastric perforation in severe malnutrition patients, suggesting timely diagnosis and management of perforation are critical to improve patient outcomes.
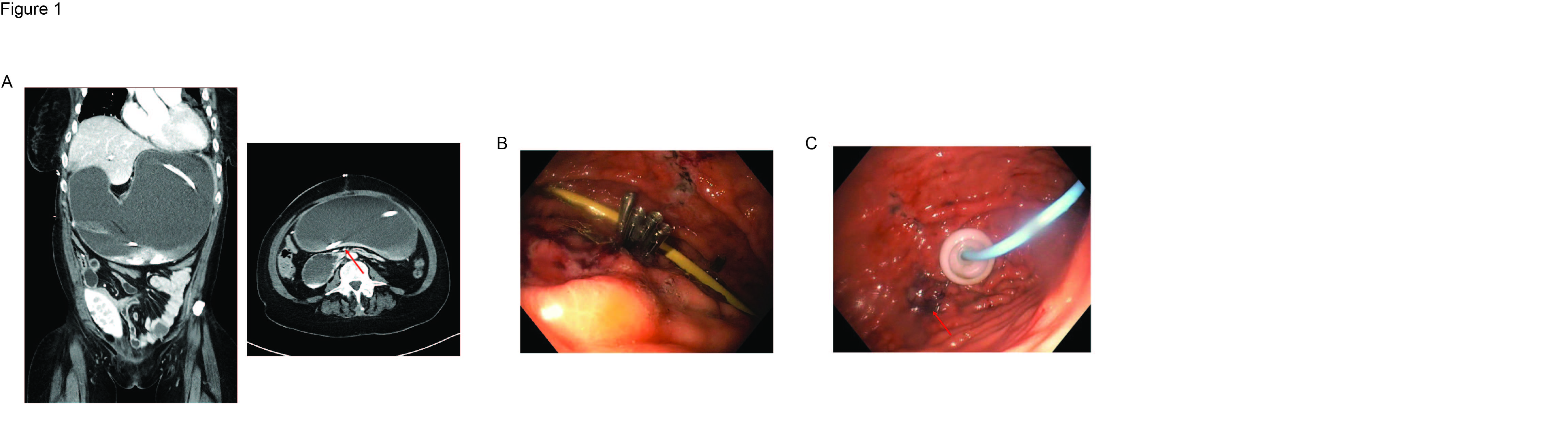
Figure: A: CT scan of abdomen at pre-procedure evaluation. Transition point of the dilation is marked as red arrow.
B: Gastroscope confirm the closure of perforation with 4 clips during the first PEG tube placement procedure.
C: At the second day PEG tube placement procedure, Gastroscope confirmation of the proper inner bumper position and gastric wall defect repairment (marked as red arrow).
B: Gastroscope confirm the closure of perforation with 4 clips during the first PEG tube placement procedure.
C: At the second day PEG tube placement procedure, Gastroscope confirmation of the proper inner bumper position and gastric wall defect repairment (marked as red arrow).
Disclosures:
Yan Yan indicated no relevant financial relationships.
Rex Siu indicated no relevant financial relationships.
Yan Bi indicated no relevant financial relationships.
Victoria Gómez: COOKMedical – Education and Lectures. Olympus – Consultant.
Vivek Kumbhari: Fujifilm – Consultant. medtronic – Consultant. microtech – Consultant.
Yuting Huang indicated no relevant financial relationships.
Yan Yan, MBBS, PhD, Rex Siu, MD, Yan Bi, MD, PhD, Victoria Gómez, MD, Vivek Kumbhari, MBChB, PhD, Yuting Huang, MBBS, PhD. P0708 - A Rare Case of Gastric Perforation During the PEG Tube Placement in a Severe Malnutrition Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
