Sunday Poster Session
Category: GI Bleeding
P0729 - Proton Pump Inhibitor Infusion Misuse and Associated Risk Factors in a Community Hospital Setting
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Harrison Pajovich, MD
Lankenau Medical Center
Philadelphia, PA
Presenting Author(s)
Harrison Pajovich, MD, Bryan Stone, MD, William Chen, MD, Stephanie Kjelstrom, MPH, Patricia Wong, MD, MSc(Epi)
Lankenau Medical Center, Wynnewood, PA
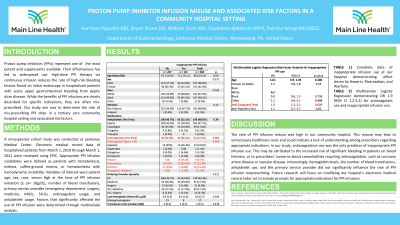
Introduction: Proton pump inhibitors (PPIs) are potent acid suppressants, and their effectiveness has led to widespread use. PPI therapy via continuous infusion reduces the rate of high-risk bleeding lesions found on initial endoscopy in hospitalized patients with acute upper gastrointestinal bleeding from peptic ulcer disease. While the benefits of PPI infusions are clearly described for specific indications, they are often mis-prescribed. Our study aim was to determine the rate of mis-prescribing PPI drips in a tertiary care community hospital and associated risk factors.
Methods: A retrospective cohort study was conducted at Lankenau Medical Center. Electronic medical record data of hospitalized patients from March 1, 2018 through March 1, 2021 were reviewed. Appropriate PPI infusion was defined as patients with hematemesis, melena, coffee-ground emesis, or hematochezia with hemodynamic instability. Variables of interest were age, sex, race, serum Hgb at the time of infusion initiation (≥ or< 10g/dL), number of transfusions, primary service (emergency, surgery, medicine, MICU, SICU), anticoagulant usage, and antiplatelet usage. Factors that significantly affected the use of PPI infusion were determined through multivariate analysis.
Results: Of 348 pre-endoscopic PPI infusions ordered during the study period, 34.8% were ordered without an appropriate indication. Anticoagulation was the only identified variable that significantly affected the rate of infusion misuse (36.4% inappropriate vs 22% appropriate [p< .005]), OR 1.9 (CI 1.2-3.2). Subgroup analysis showed an increased risk of PPI infusion misuse in patients who were on warfarin, heparin, enoxaparin, and rivaroxaban (p< 0.005) and no significant risk in patients who were on apixaban, dabigatran, or argatroban.
Discussion: The high rate of PPI infusion misuse in our community hospital may lead to unnecessary costs and may reflect a lack of understanding of appropriate indications. Anticoagulation use was the only predictor of inappropriate use in our study. This may be due to the increased risk of significant bleeding among patients who are on blood thinners or concern about comorbidities in patients that require anticoagulation such as coronary or vascular disease. Interestingly, hemoglobin value, number of transfusions, antiplatelet usage, and primary service provider did not significantly affect the rate of misuse. A future study will focus on a modified electronic medical record orderset to prompt appropriate indications for PPI infusions.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Harrison Pajovich, MD, Bryan Stone, MD, William Chen, MD, Stephanie Kjelstrom, MPH, Patricia Wong, MD, MSc(Epi). P0729 - Proton Pump Inhibitor Infusion Misuse and Associated Risk Factors in a Community Hospital Setting, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Lankenau Medical Center, Wynnewood, PA
Introduction: Proton pump inhibitors (PPIs) are potent acid suppressants, and their effectiveness has led to widespread use. PPI therapy via continuous infusion reduces the rate of high-risk bleeding lesions found on initial endoscopy in hospitalized patients with acute upper gastrointestinal bleeding from peptic ulcer disease. While the benefits of PPI infusions are clearly described for specific indications, they are often mis-prescribed. Our study aim was to determine the rate of mis-prescribing PPI drips in a tertiary care community hospital and associated risk factors.
Methods: A retrospective cohort study was conducted at Lankenau Medical Center. Electronic medical record data of hospitalized patients from March 1, 2018 through March 1, 2021 were reviewed. Appropriate PPI infusion was defined as patients with hematemesis, melena, coffee-ground emesis, or hematochezia with hemodynamic instability. Variables of interest were age, sex, race, serum Hgb at the time of infusion initiation (≥ or< 10g/dL), number of transfusions, primary service (emergency, surgery, medicine, MICU, SICU), anticoagulant usage, and antiplatelet usage. Factors that significantly affected the use of PPI infusion were determined through multivariate analysis.
Results: Of 348 pre-endoscopic PPI infusions ordered during the study period, 34.8% were ordered without an appropriate indication. Anticoagulation was the only identified variable that significantly affected the rate of infusion misuse (36.4% inappropriate vs 22% appropriate [p< .005]), OR 1.9 (CI 1.2-3.2). Subgroup analysis showed an increased risk of PPI infusion misuse in patients who were on warfarin, heparin, enoxaparin, and rivaroxaban (p< 0.005) and no significant risk in patients who were on apixaban, dabigatran, or argatroban.
Discussion: The high rate of PPI infusion misuse in our community hospital may lead to unnecessary costs and may reflect a lack of understanding of appropriate indications. Anticoagulation use was the only predictor of inappropriate use in our study. This may be due to the increased risk of significant bleeding among patients who are on blood thinners or concern about comorbidities in patients that require anticoagulation such as coronary or vascular disease. Interestingly, hemoglobin value, number of transfusions, antiplatelet usage, and primary service provider did not significantly affect the rate of misuse. A future study will focus on a modified electronic medical record orderset to prompt appropriate indications for PPI infusions.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Harrison Pajovich indicated no relevant financial relationships.
Bryan Stone indicated no relevant financial relationships.
William Chen indicated no relevant financial relationships.
Stephanie Kjelstrom indicated no relevant financial relationships.
Patricia Wong indicated no relevant financial relationships.
Harrison Pajovich, MD, Bryan Stone, MD, William Chen, MD, Stephanie Kjelstrom, MPH, Patricia Wong, MD, MSc(Epi). P0729 - Proton Pump Inhibitor Infusion Misuse and Associated Risk Factors in a Community Hospital Setting, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
