Sunday Poster Session
Category: GI Bleeding
P0733 - Navigating Barriers: Bridging Gaps in Secondary Prevention for Gastroesophogeal Variceal Bleeding in Cirrhotic Patients
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
Dakota Bigham, MD
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Dakota Bigham, MD1, Adam Vinall, MD2, Fatma Ozguc, DO3, Benjamin Heriford, DO3, James Alvarez, MD3, Keerthi Thallapureddy, MD1, Jawairia Memon, MD2
1University of Texas Health San Antonio, San Antonio, TX; 2University of Texas Health Science Center, San Antonio, TX; 3UTHSCSA, San Antonio, TX
Introduction: Gastroesophageal varices represent a common complication of cirrhosis, stemming from heightened portal pressures. Variceal bleeding poses a life-threatening risk and significantly elevates mortality rates in cirrhotic patients. Despite guidelines advocating for nonselective beta blockers and surveillance endoscopy following variceal bleeding, research indicates a notable underutilization of secondary prevention strategies by clinicians.
Methods: This retrospective observational study examines patients with variceal bleeding treated at an inpatient university hospital from 2022 to 2023. Primary inclusion criteria encompassed patients aged over 18 who were hospitalized with an ICD code indicating esophageal variceal bleeding. Subsequent evaluation focused on ICU admission, the requirement for TIPS, discharge with beta blockers for secondary prophylaxis, and rates of follow-up EGD.
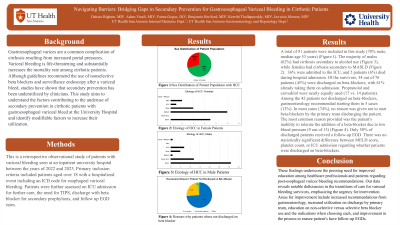
Results: A total of 81 patients were included in this study (70% male, median age 53 years). The majority (62%) had cirrhosis secondary to alcohol use, 36% were admitted to the ICU, and 5 patients (6%) died during hospital admission. Of the survivors, 34 out of 76 patients (45%) were discharged on beta-blockers, with 61% already taking them on admission. Propranolol and carvedilol were nearly equally used (17 vs. 14 patients). Among the 42 patients not discharged on beta-blockers, gastroenterology recommended starting them in 5 cases (12%). In most cases (74%), no reason was given not to start beta-blockers by the primary team discharging the patient. The most common reason provided was the patient's inability to tolerate the addition of a beta-blocker due to low blood pressure (9 out of 13). Only 50% of discharged patients received a follow-up EGD. There was no statistically significant difference between MELD score, platelet count, or ICU admission regarding whether patients were discharged on beta-blockers.
Discussion: These findings highlight the urgent requirement for enhanced education among healthcare professionals and patients concerning post-esophageal variceal bleeding recommendations. Our data exposes significant shortcomings in the transitional care provided to variceal bleeding survivors, underscoring the ugency for intervention. Areas necessitating improvement encompass heightened recommendations from gastroenterology, augmented utilization by the primary team upon discharge, and enhancement of the process to ensure patients undergo follow-up EGDs.
Disclosures:
Dakota Bigham, MD1, Adam Vinall, MD2, Fatma Ozguc, DO3, Benjamin Heriford, DO3, James Alvarez, MD3, Keerthi Thallapureddy, MD1, Jawairia Memon, MD2. P0733 - Navigating Barriers: Bridging Gaps in Secondary Prevention for Gastroesophogeal Variceal Bleeding in Cirrhotic Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health San Antonio, San Antonio, TX; 2University of Texas Health Science Center, San Antonio, TX; 3UTHSCSA, San Antonio, TX
Introduction: Gastroesophageal varices represent a common complication of cirrhosis, stemming from heightened portal pressures. Variceal bleeding poses a life-threatening risk and significantly elevates mortality rates in cirrhotic patients. Despite guidelines advocating for nonselective beta blockers and surveillance endoscopy following variceal bleeding, research indicates a notable underutilization of secondary prevention strategies by clinicians.
Methods: This retrospective observational study examines patients with variceal bleeding treated at an inpatient university hospital from 2022 to 2023. Primary inclusion criteria encompassed patients aged over 18 who were hospitalized with an ICD code indicating esophageal variceal bleeding. Subsequent evaluation focused on ICU admission, the requirement for TIPS, discharge with beta blockers for secondary prophylaxis, and rates of follow-up EGD.
Results: A total of 81 patients were included in this study (70% male, median age 53 years). The majority (62%) had cirrhosis secondary to alcohol use, 36% were admitted to the ICU, and 5 patients (6%) died during hospital admission. Of the survivors, 34 out of 76 patients (45%) were discharged on beta-blockers, with 61% already taking them on admission. Propranolol and carvedilol were nearly equally used (17 vs. 14 patients). Among the 42 patients not discharged on beta-blockers, gastroenterology recommended starting them in 5 cases (12%). In most cases (74%), no reason was given not to start beta-blockers by the primary team discharging the patient. The most common reason provided was the patient's inability to tolerate the addition of a beta-blocker due to low blood pressure (9 out of 13). Only 50% of discharged patients received a follow-up EGD. There was no statistically significant difference between MELD score, platelet count, or ICU admission regarding whether patients were discharged on beta-blockers.
Discussion: These findings highlight the urgent requirement for enhanced education among healthcare professionals and patients concerning post-esophageal variceal bleeding recommendations. Our data exposes significant shortcomings in the transitional care provided to variceal bleeding survivors, underscoring the ugency for intervention. Areas necessitating improvement encompass heightened recommendations from gastroenterology, augmented utilization by the primary team upon discharge, and enhancement of the process to ensure patients undergo follow-up EGDs.
Disclosures:
Dakota Bigham indicated no relevant financial relationships.
Adam Vinall indicated no relevant financial relationships.
Fatma Ozguc indicated no relevant financial relationships.
Benjamin Heriford indicated no relevant financial relationships.
James Alvarez indicated no relevant financial relationships.
Keerthi Thallapureddy indicated no relevant financial relationships.
Jawairia Memon indicated no relevant financial relationships.
Dakota Bigham, MD1, Adam Vinall, MD2, Fatma Ozguc, DO3, Benjamin Heriford, DO3, James Alvarez, MD3, Keerthi Thallapureddy, MD1, Jawairia Memon, MD2. P0733 - Navigating Barriers: Bridging Gaps in Secondary Prevention for Gastroesophogeal Variceal Bleeding in Cirrhotic Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
