Sunday Poster Session
Category: GI Bleeding
P0736 - Outcomes of Upper Gastrointestinal Bleeding in Puerto Rico: Did the COVID-19 Pandemic Make It Worse?
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Ana Maria Davila, MD
Rush University Medical Center
Chicago, IL
Presenting Author(s)
Ana Maria Davila, MD1, Pablo Costas, MD2, Christopher Chapman, BS3
1Rush University Medical Center, Chicago, IL; 2University of Puerto Rico, Medical Sciences Campus, San Juan, Puerto Rico; 3University of Puerto Rico School of Medicine, San Juan, Puerto Rico
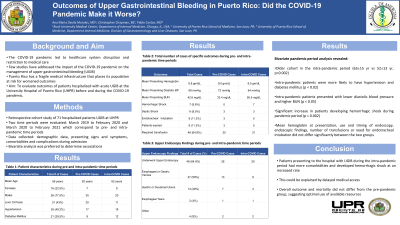
Introduction: The COVID-19 pandemic led to significant healthcare system disruption mainly by restricting access to medical care. Few studies have addressed the impact of the COVID-19 pandemic on the management of upper gastrointestinal bleeding (UGIB). We sought to identify the outcomes of patients hospitalized with acute UGIB at the University Hospital of the Puerto Rico (UHPR) given the island’s fragile medical infrastructure and high risk for worsened outcomes.
Methods: A retrospective cohort study of 71 patients hospitalized for UGIB at the UHPR was performed during two time periods: March 1, 2019 to February 29, 2020 and March 1, 2020 to March 1, 2021 corresponding to pre- and intra-pandemic time periods. Demographic data, presenting signs and symptoms, comorbidities and complications during admission were obtained and bivariate analysis was performed.
Results: Seventy-one hospital charts were reviewed. Sixteen patients were women (22.5%). Mean age was 56 years and 31 subjects (43%) had liver cirrhosis. Mean Hgb at presentation was 8.8 gm/dl and mean platelet count was 220,000 /μL. Seven patients developed hemorrhagic shock, 6 developed septic shock and 8 required endotracheal intubation. Eight patients died (11%). Forty-six patients required transfusion of at least one unit of packed red blood cells (65%). Forty-six patients underwent upper endoscopy (65%) with the following findings: 27 esophageal or gastric varices (59% of all endoscopies), all of which were treated with variceal ligation, 13 gastric or duodenal ulcers (28%), 2 esophageal tears (4%), and other diagnoses (9%). Bivariate pandemic period analysis revealed an older cohort in the intra-pandemic period (63±15 yr vs 52±13 yr, p=0.002). Intra-pandemic patients were more likely to have hypertension and diabetes mellitus (p < 0.02) and present with lower diastolic blood pressure and higher BUN (p < 0.05). During the pandemic period, there was a significant increase in patients developing hemorrhagic shock (p = 0.002). Mean Hgb at presentation, use and timing of endoscopy, endoscopic findings, transfusions, or need for endotracheal intubation did not differ significantly between the two groups.
Discussion: Patients presenting to the hospital with UGIB during the intra-pandemic period had more comorbidities and developed hemorrhagic shock at an increased rate, which could be explained by delayed medical access. However, overall outcome and mortality did not differ from the pre-pandemic group, suggesting optimal use of available resources.
Disclosures:
Ana Maria Davila, MD1, Pablo Costas, MD2, Christopher Chapman, BS3. P0736 - Outcomes of Upper Gastrointestinal Bleeding in Puerto Rico: Did the COVID-19 Pandemic Make It Worse?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Rush University Medical Center, Chicago, IL; 2University of Puerto Rico, Medical Sciences Campus, San Juan, Puerto Rico; 3University of Puerto Rico School of Medicine, San Juan, Puerto Rico
Introduction: The COVID-19 pandemic led to significant healthcare system disruption mainly by restricting access to medical care. Few studies have addressed the impact of the COVID-19 pandemic on the management of upper gastrointestinal bleeding (UGIB). We sought to identify the outcomes of patients hospitalized with acute UGIB at the University Hospital of the Puerto Rico (UHPR) given the island’s fragile medical infrastructure and high risk for worsened outcomes.
Methods: A retrospective cohort study of 71 patients hospitalized for UGIB at the UHPR was performed during two time periods: March 1, 2019 to February 29, 2020 and March 1, 2020 to March 1, 2021 corresponding to pre- and intra-pandemic time periods. Demographic data, presenting signs and symptoms, comorbidities and complications during admission were obtained and bivariate analysis was performed.
Results: Seventy-one hospital charts were reviewed. Sixteen patients were women (22.5%). Mean age was 56 years and 31 subjects (43%) had liver cirrhosis. Mean Hgb at presentation was 8.8 gm/dl and mean platelet count was 220,000 /μL. Seven patients developed hemorrhagic shock, 6 developed septic shock and 8 required endotracheal intubation. Eight patients died (11%). Forty-six patients required transfusion of at least one unit of packed red blood cells (65%). Forty-six patients underwent upper endoscopy (65%) with the following findings: 27 esophageal or gastric varices (59% of all endoscopies), all of which were treated with variceal ligation, 13 gastric or duodenal ulcers (28%), 2 esophageal tears (4%), and other diagnoses (9%). Bivariate pandemic period analysis revealed an older cohort in the intra-pandemic period (63±15 yr vs 52±13 yr, p=0.002). Intra-pandemic patients were more likely to have hypertension and diabetes mellitus (p < 0.02) and present with lower diastolic blood pressure and higher BUN (p < 0.05). During the pandemic period, there was a significant increase in patients developing hemorrhagic shock (p = 0.002). Mean Hgb at presentation, use and timing of endoscopy, endoscopic findings, transfusions, or need for endotracheal intubation did not differ significantly between the two groups.
Discussion: Patients presenting to the hospital with UGIB during the intra-pandemic period had more comorbidities and developed hemorrhagic shock at an increased rate, which could be explained by delayed medical access. However, overall outcome and mortality did not differ from the pre-pandemic group, suggesting optimal use of available resources.
Disclosures:
Ana Maria Davila indicated no relevant financial relationships.
Pablo Costas indicated no relevant financial relationships.
Christopher Chapman indicated no relevant financial relationships.
Ana Maria Davila, MD1, Pablo Costas, MD2, Christopher Chapman, BS3. P0736 - Outcomes of Upper Gastrointestinal Bleeding in Puerto Rico: Did the COVID-19 Pandemic Make It Worse?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
