Sunday Poster Session
Category: GI Bleeding
P0737 - Endoscopic Interventions: Clinical Impact on Outcomes in Patients With Post-Percutaneous Coronary Interventions Gastrointestinal Bleeding: A Retrospective Single Center Cohort Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E

Pratiksha Moliya, MD
Jamaica Hospital Medical Center
Edison, NJ
Presenting Author(s)
Pratiksha Moliya, MD1, Hasan Al-Obaidi, MD2, Joseph Joseph, MD3, Srikaran Bojja, MD4, Asit Mehta, MD5
1Jamaica Hospital Medical Center, Edison, NJ; 2Jamaica Hospital Medical Center, Briarwood, NY; 3Jamaica Hospital Medical Center, Queens, NY; 4BronxCare Health System, Bronx, NY; 5Jamaica Hospital Medical Center, New York, NY
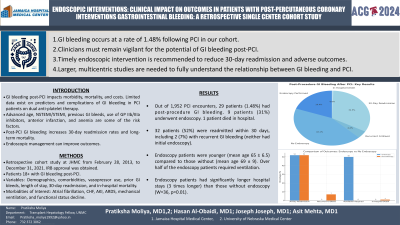
Introduction: Gastrointestinal(GI) bleeding significantly impacts morbidity, mortality, and economic costs. Limited data are available on the predictors and complications of GI bleeding amongst patients treated with primary Percutaneous Coronary Intervention(PCI) and dual antiplatelet therapy. Among ACS patients undergoing PCI, the risk of GI bleeding is related to a number of risk factors, including advanced age, NSTEMI/STEMI, previous GI bleeds, GP IIB/IIIA inhibitors, anterior infarction and anemia.The available literature shows post-PCI GI bleeding, though rare, leads to higher 30-day readmission and increased long-term mortality. Endoscopic management can improve outcomes.
Methods: This IRB study aims to examine the risk factors, treatment differences, and negative outcomes—such as morbidity, mortality, and 30-day readmission—among patients experiencing GI bleeding post-PCI in a community hospital setting. Retrospective cohort study of patients (18+ years) admitted to JHMC hospital between February 28, 2013, and December 31, 2021, diagnosed with GI bleeding post-PCI. Variables include demographics, comorbidities, vasopressor use, previous GI bleeds, hospitalization duration, 30-day readmission, and in-hospital mortality. Specific morbidities of interest are atrial fibrillation, CHF, AKI, ARDS, mechanical ventilation, and decreased functional status from baseline.
Results: From 1,952 PCI encounters, 29 patients were identified with post-procedure GI bleeding. Of these, 9 (31%) underwent endoscopy. One patient died in hospital, and 32 (52%) were readmitted within 30 days, including 2 (7%) with recurrent GI bleeding; neither had initial endoscopy. Endoscopy patients were younger (mean age 65 ± 6.5) than those without (mean age 69 ± 9), and over half required ventilation. Significant differences in hospital stay length were noted; endoscopy patients stayed three times longer than those without endoscopy (W=36, p=0.01).
Discussion: In conclusion, our study shows that GI bleeding occurs at a rate of 1.48% following PCI in our cohort. This highlights the need for clinicians to remain vigilant about the potential for GI bleeding post-PCI. To reduce the risk of 30-day readmission and other adverse outcomes, timely endoscopic intervention should be considered for those experiencing GI bleeding after PCI. However, to fully understand the relationship between GI bleeding and PCI, more comprehensive analyses with larger, diverse study groups and multicentric studies are essential.
Disclosures:
Pratiksha Moliya, MD1, Hasan Al-Obaidi, MD2, Joseph Joseph, MD3, Srikaran Bojja, MD4, Asit Mehta, MD5. P0737 - Endoscopic Interventions: Clinical Impact on Outcomes in Patients With Post-Percutaneous Coronary Interventions Gastrointestinal Bleeding: A Retrospective Single Center Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Jamaica Hospital Medical Center, Edison, NJ; 2Jamaica Hospital Medical Center, Briarwood, NY; 3Jamaica Hospital Medical Center, Queens, NY; 4BronxCare Health System, Bronx, NY; 5Jamaica Hospital Medical Center, New York, NY
Introduction: Gastrointestinal(GI) bleeding significantly impacts morbidity, mortality, and economic costs. Limited data are available on the predictors and complications of GI bleeding amongst patients treated with primary Percutaneous Coronary Intervention(PCI) and dual antiplatelet therapy. Among ACS patients undergoing PCI, the risk of GI bleeding is related to a number of risk factors, including advanced age, NSTEMI/STEMI, previous GI bleeds, GP IIB/IIIA inhibitors, anterior infarction and anemia.The available literature shows post-PCI GI bleeding, though rare, leads to higher 30-day readmission and increased long-term mortality. Endoscopic management can improve outcomes.
Methods: This IRB study aims to examine the risk factors, treatment differences, and negative outcomes—such as morbidity, mortality, and 30-day readmission—among patients experiencing GI bleeding post-PCI in a community hospital setting. Retrospective cohort study of patients (18+ years) admitted to JHMC hospital between February 28, 2013, and December 31, 2021, diagnosed with GI bleeding post-PCI. Variables include demographics, comorbidities, vasopressor use, previous GI bleeds, hospitalization duration, 30-day readmission, and in-hospital mortality. Specific morbidities of interest are atrial fibrillation, CHF, AKI, ARDS, mechanical ventilation, and decreased functional status from baseline.
Results: From 1,952 PCI encounters, 29 patients were identified with post-procedure GI bleeding. Of these, 9 (31%) underwent endoscopy. One patient died in hospital, and 32 (52%) were readmitted within 30 days, including 2 (7%) with recurrent GI bleeding; neither had initial endoscopy. Endoscopy patients were younger (mean age 65 ± 6.5) than those without (mean age 69 ± 9), and over half required ventilation. Significant differences in hospital stay length were noted; endoscopy patients stayed three times longer than those without endoscopy (W=36, p=0.01).
Discussion: In conclusion, our study shows that GI bleeding occurs at a rate of 1.48% following PCI in our cohort. This highlights the need for clinicians to remain vigilant about the potential for GI bleeding post-PCI. To reduce the risk of 30-day readmission and other adverse outcomes, timely endoscopic intervention should be considered for those experiencing GI bleeding after PCI. However, to fully understand the relationship between GI bleeding and PCI, more comprehensive analyses with larger, diverse study groups and multicentric studies are essential.
Disclosures:
Pratiksha Moliya indicated no relevant financial relationships.
Hasan Al-Obaidi indicated no relevant financial relationships.
Joseph Joseph indicated no relevant financial relationships.
Srikaran Bojja indicated no relevant financial relationships.
Asit Mehta indicated no relevant financial relationships.
Pratiksha Moliya, MD1, Hasan Al-Obaidi, MD2, Joseph Joseph, MD3, Srikaran Bojja, MD4, Asit Mehta, MD5. P0737 - Endoscopic Interventions: Clinical Impact on Outcomes in Patients With Post-Percutaneous Coronary Interventions Gastrointestinal Bleeding: A Retrospective Single Center Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
