Sunday Poster Session
Category: GI Bleeding
P0738 - Gastrointestinal Bleeding Simulation Improves Resident Knowledge and Confidence
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Marni H. Wilkoff, DO
Mount Sinai Morningside/West
New York, NY
Presenting Author(s)
Marni H. Wilkoff, DO1, Emily Seltzer, DO2, Nicholas R. Piniella, DO, MS3, Harrindra Seepersaud, PhD, MPH, MA, MS2, Priscilla Loanzon, RN2, Susannah Kurtz, MD2, James Salonia, MD2, Daniela Jodorkovsky, MD4
1Mount Sinai Morningside/West, New York, NY; 2Mount Sinai West, New York, NY; 3New York Institute of Technology College of Osteopathic Medicine, New Jersey, NJ; 4Mount Sinai Center for Gastrointestinal Physiology & Motility, New York, NY
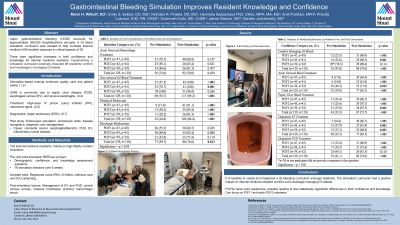
Introduction: Upper gastrointestinal (GI) bleeding from peptic ulcer disease (PUD), esophageal varices (EV), or erosive esophagitis, account for approximately 350,000 admissions annually. Simulation-based training is a popular medical education tool, with enhancement of quality care and patient safety, and can help learners recognize a disease process, initiate proper workup, and treatment. To increase internal medicine (IM) resident exposure to critical aspects of GI, a GI bleed simulation curriculum was created.
Methods: One hundred and twenty-nine IM residents, split into 16 groups, participated in a 1-hour hands-on high-fidelity manikin simulation. Pre- and post-simulation REDCap surveys were distributed and included demographic, confidence scale, and knowledge assessment questions. A case outline included a narrative description, learning objectives, critical actions, history of present illness, vital signs, and physical exam. Participants encountered a patient with a past medical history of alcohol use disorder presenting to the emergency department with abdominal pain and swelling. A rapid response was called 12hrs after admission for hematemesis and hemodynamic instability. Progression of the case was detailed with changing vital signs, exam findings and labs. Key equipment included a high-fidelity manikin, code cart, introducer kit, and moulage hematemesis and melena. A post-simulation debrief focused on inpatient and outpatient management of EV and PUD, central venous access, massive transfusion protocol, and hemorrhagic shock.
Results: There was a significant increase in the level of confidence for interns (PGY1) and second year (PGY2) residents in all categories (p < .05). Third year (PGY3) residents had a significant increase in confidence in managing acute variceal bleeds (p = 0.03), peptic ulcer bleeding (p = 0.002), and outpatient EV (p = 0.003).
There was a significant increase in PGY1 and PGY2 knowledge on treatment of non-variceal GI bleeds (p = < .001, p = 0.001). All residents had a significant increase in their knowledge of timing of endoscopy for acute EV bleeds (p < .001). Among all residents combined, there was a statistically significant increase in knowledge of discharge medications for EV and PUD (p = 0.01).
Discussion: Simulation is a prevalent tool used in medical education. This study showed that implementation of a hands-on manikin simulation has a positive impact on IM resident comfort and knowledge managing GI bleeds.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Marni H. Wilkoff, DO1, Emily Seltzer, DO2, Nicholas R. Piniella, DO, MS3, Harrindra Seepersaud, PhD, MPH, MA, MS2, Priscilla Loanzon, RN2, Susannah Kurtz, MD2, James Salonia, MD2, Daniela Jodorkovsky, MD4. P0738 - Gastrointestinal Bleeding Simulation Improves Resident Knowledge and Confidence, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mount Sinai Morningside/West, New York, NY; 2Mount Sinai West, New York, NY; 3New York Institute of Technology College of Osteopathic Medicine, New Jersey, NJ; 4Mount Sinai Center for Gastrointestinal Physiology & Motility, New York, NY
Introduction: Upper gastrointestinal (GI) bleeding from peptic ulcer disease (PUD), esophageal varices (EV), or erosive esophagitis, account for approximately 350,000 admissions annually. Simulation-based training is a popular medical education tool, with enhancement of quality care and patient safety, and can help learners recognize a disease process, initiate proper workup, and treatment. To increase internal medicine (IM) resident exposure to critical aspects of GI, a GI bleed simulation curriculum was created.
Methods: One hundred and twenty-nine IM residents, split into 16 groups, participated in a 1-hour hands-on high-fidelity manikin simulation. Pre- and post-simulation REDCap surveys were distributed and included demographic, confidence scale, and knowledge assessment questions. A case outline included a narrative description, learning objectives, critical actions, history of present illness, vital signs, and physical exam. Participants encountered a patient with a past medical history of alcohol use disorder presenting to the emergency department with abdominal pain and swelling. A rapid response was called 12hrs after admission for hematemesis and hemodynamic instability. Progression of the case was detailed with changing vital signs, exam findings and labs. Key equipment included a high-fidelity manikin, code cart, introducer kit, and moulage hematemesis and melena. A post-simulation debrief focused on inpatient and outpatient management of EV and PUD, central venous access, massive transfusion protocol, and hemorrhagic shock.
Results: There was a significant increase in the level of confidence for interns (PGY1) and second year (PGY2) residents in all categories (p < .05). Third year (PGY3) residents had a significant increase in confidence in managing acute variceal bleeds (p = 0.03), peptic ulcer bleeding (p = 0.002), and outpatient EV (p = 0.003).
There was a significant increase in PGY1 and PGY2 knowledge on treatment of non-variceal GI bleeds (p = < .001, p = 0.001). All residents had a significant increase in their knowledge of timing of endoscopy for acute EV bleeds (p < .001). Among all residents combined, there was a statistically significant increase in knowledge of discharge medications for EV and PUD (p = 0.01).
Discussion: Simulation is a prevalent tool used in medical education. This study showed that implementation of a hands-on manikin simulation has a positive impact on IM resident comfort and knowledge managing GI bleeds.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Marni Wilkoff indicated no relevant financial relationships.
Emily Seltzer indicated no relevant financial relationships.
Nicholas Piniella indicated no relevant financial relationships.
Harrindra Seepersaud indicated no relevant financial relationships.
Priscilla Loanzon indicated no relevant financial relationships.
Susannah Kurtz indicated no relevant financial relationships.
James Salonia indicated no relevant financial relationships.
Daniela Jodorkovsky: Atmo Biosciences – Consultant.
Marni H. Wilkoff, DO1, Emily Seltzer, DO2, Nicholas R. Piniella, DO, MS3, Harrindra Seepersaud, PhD, MPH, MA, MS2, Priscilla Loanzon, RN2, Susannah Kurtz, MD2, James Salonia, MD2, Daniela Jodorkovsky, MD4. P0738 - Gastrointestinal Bleeding Simulation Improves Resident Knowledge and Confidence, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

