Sunday Poster Session
Category: GI Bleeding
P0745 - A Closer Look into Gastrointestinal Bleeding in Heart Failure Patients
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- AZ
Anas Zaher, MD
New York-Presbyterian / Brooklyn Methodist Hospital
Brooklyn, NY
Presenting Author(s)
Anas Zaher, MD1, Jude Elsaygh, MD1, Akram Midani, MD1, Andrew Treihaft, MD1, Brinda Banerji, MD1, Muhammad F. Bouso, MD1, Malik Mushannen, MD1, Rawan Hussein, MD1, Carl V. Crawford, MD2
1New York-Presbyterian / Brooklyn Methodist Hospital, Brooklyn, NY; 2New York-Presbyterian / Weill Cornell Medical Center, New York, NY
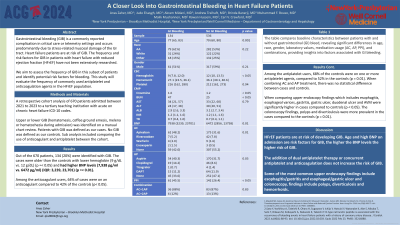
Introduction: The frequency and risk factors for gastrointestinal bleed (GIB) in patients with heart failure with reduced ejection fraction (HFrEF) have not been extensively researched. We aim to assess the frequency of GIB in this subset of patients and identify potential risk factors for bleeding. This study will evaluate the frequency of commonly used antiplatelet and anticoagulation agents in the HFrEF population.
Methods: A retrospective cohort analysis of 670 patients admitted between 11/2021 to 08/2023 to a tertiary teaching institution with acute on chronic heart failure ICD-10 codes. Upper or lower GIB (hematemesis, coffee ground emesis, melena or hematochezia during admission) was identified on a manual chart review. Patients with GIB was defined as our cases. No GIB was defined as our controls. Sub analysis included comparing the use of anticoagulant and antiplatelet between the cohort. Independent t test assessed statistical differences in the case and control groups.
Results: Out of the 670 patients, 134 (20%) were identified with GIB. The cases were older than the controls with lower hemoglobin (9 g/dL vs. 12 g/dL) (p =< 0.05) and had higher BNP levels (7,938 pg/ml vs. 6472 pg/ml) (IQR: 3,239, 23,701) (p =< 0.01). Among the anticoagulant users, 64% of cases were on an anticoagulant compared to 42% of the controls (p< 0.05). Among the antiplatelet users, 68% of the controls were on one or more antiplatelet agents, compared to 52% in the controls (p = 0.01). When combining AC and AP treatment, there was no statistical difference between cases and controls. Ninety-three (69%) patients from cases had cross-sectional imaging with only 25% showing abnormal findings like diverticulosis, colitis, and masses. When comparing upper endoscopy findings which includes esophagitis, esophageal varices, gastritis, gastric ulcer, duodenal ulcer and AVM were significantly higher in cases compared to controls (p < 0.05). T he colonoscopy findings, polyps and diverticulosis were more prevalent in the cases compared to the controls (p = 0.01).
Discussion: HFrEF patients are at risk of developing GIB. Age and high BNP on admission are risk factors for GIB, the higher the BNP levels the higher risk of GIB. The addition of dual antiplatelet therapy or concurrent antiplatelet and anticoagulation does not increase the risk of GIB. Some of the most common upper endoscopy findings include esophagitis/gastritis and esophageal/gastric ulcer and colonoscopy, findings include polyps, diverticulosis and hemorrhoids.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Anas Zaher, MD1, Jude Elsaygh, MD1, Akram Midani, MD1, Andrew Treihaft, MD1, Brinda Banerji, MD1, Muhammad F. Bouso, MD1, Malik Mushannen, MD1, Rawan Hussein, MD1, Carl V. Crawford, MD2. P0745 - A Closer Look into Gastrointestinal Bleeding in Heart Failure Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York-Presbyterian / Brooklyn Methodist Hospital, Brooklyn, NY; 2New York-Presbyterian / Weill Cornell Medical Center, New York, NY
Introduction: The frequency and risk factors for gastrointestinal bleed (GIB) in patients with heart failure with reduced ejection fraction (HFrEF) have not been extensively researched. We aim to assess the frequency of GIB in this subset of patients and identify potential risk factors for bleeding. This study will evaluate the frequency of commonly used antiplatelet and anticoagulation agents in the HFrEF population.
Methods: A retrospective cohort analysis of 670 patients admitted between 11/2021 to 08/2023 to a tertiary teaching institution with acute on chronic heart failure ICD-10 codes. Upper or lower GIB (hematemesis, coffee ground emesis, melena or hematochezia during admission) was identified on a manual chart review. Patients with GIB was defined as our cases. No GIB was defined as our controls. Sub analysis included comparing the use of anticoagulant and antiplatelet between the cohort. Independent t test assessed statistical differences in the case and control groups.
Results: Out of the 670 patients, 134 (20%) were identified with GIB. The cases were older than the controls with lower hemoglobin (9 g/dL vs. 12 g/dL) (p =< 0.05) and had higher BNP levels (7,938 pg/ml vs. 6472 pg/ml) (IQR: 3,239, 23,701) (p =< 0.01). Among the anticoagulant users, 64% of cases were on an anticoagulant compared to 42% of the controls (p< 0.05). Among the antiplatelet users, 68% of the controls were on one or more antiplatelet agents, compared to 52% in the controls (p = 0.01). When combining AC and AP treatment, there was no statistical difference between cases and controls. Ninety-three (69%) patients from cases had cross-sectional imaging with only 25% showing abnormal findings like diverticulosis, colitis, and masses. When comparing upper endoscopy findings which includes esophagitis, esophageal varices, gastritis, gastric ulcer, duodenal ulcer and AVM were significantly higher in cases compared to controls (p < 0.05). T he colonoscopy findings, polyps and diverticulosis were more prevalent in the cases compared to the controls (p = 0.01).
Discussion: HFrEF patients are at risk of developing GIB. Age and high BNP on admission are risk factors for GIB, the higher the BNP levels the higher risk of GIB. The addition of dual antiplatelet therapy or concurrent antiplatelet and anticoagulation does not increase the risk of GIB. Some of the most common upper endoscopy findings include esophagitis/gastritis and esophageal/gastric ulcer and colonoscopy, findings include polyps, diverticulosis and hemorrhoids.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Anas Zaher indicated no relevant financial relationships.
Jude Elsaygh indicated no relevant financial relationships.
Akram Midani indicated no relevant financial relationships.
Andrew Treihaft indicated no relevant financial relationships.
Brinda Banerji indicated no relevant financial relationships.
Muhammad Bouso indicated no relevant financial relationships.
Malik Mushannen indicated no relevant financial relationships.
Rawan Hussein indicated no relevant financial relationships.
Carl Crawford: Ferring – Grant/Research Support. Nestle – Speakers Bureau. Phathom – Speakers Bureau. Seres – Speakers Bureau. Vedanta – Grant/Research Support.
Anas Zaher, MD1, Jude Elsaygh, MD1, Akram Midani, MD1, Andrew Treihaft, MD1, Brinda Banerji, MD1, Muhammad F. Bouso, MD1, Malik Mushannen, MD1, Rawan Hussein, MD1, Carl V. Crawford, MD2. P0745 - A Closer Look into Gastrointestinal Bleeding in Heart Failure Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
