Sunday Poster Session
Category: GI Bleeding
P0773 - Peristomal Pseudoaneurysm Presenting as Blood in Colostomy Bag
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- AP
Arjun Ponduri, MD
Valley Hospital Medical Center
Las Vegas, NV
Presenting Author(s)
Arjun Ponduri, MD, Elen Sarkisyan, DO, Scott Diamond, DO, Vishvinder Sharma, MD
Valley Hospital Medical Center, Las Vegas, NV
Introduction: A pseudoaneurysm results from vascular injury and results in hemorrhage and adjacent hematoma. This is primarily the result of medical procedures such as angiograms and cardiac catheterizations but also often result from severe pancreatitis presenting as a GI bleed. Complications from pseudoaneurysms include rupture and hemorrhage. Rupture rates can be between 2-45% based on the location of the pseudoaneurysm. Mortality rates of hemorrhage range between 12.5-37%, with important risk factors including age and hypertension. We present a case of a patient who presented with frank blood in his colostomy bag from a hemorrhaging peristomal pseudoaneurysm.
Case Description/Methods: A 49 year old male had a history of severe, acute pancreatitis 17 months prior complicated by a colon perforation requiring an ex- lap with distal pancreatectomy and a left hemicolectomy with colostomy. He presented with bloody output in his colostomy bag. Patient also noted generalized abdominal pain around the colostomy bag.
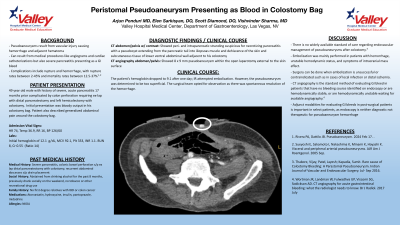
Hemoglobin on admission was 12.1. A CT of the abdomen and pelvis with IV contrast showed peri- and intrapancreatic stranding suspicious for necrotizing pancreatitis with a pseudocyst extending from the pancreatic tail into iliopsoas muscle and dehiscence of the skin and subcutaneous tissue of lower ventral abdominal wall adjacent to his colostomy.
A CT angiography of the abdomen/pelvis was ordered revealing an 8 x 9 mm pseudoaneurysm within the open laparotomy external to the skin surface.
The patient’s hemoglobin dropped to 9.1 and IR attempted embolization; however it was too superficial. The surgical team opted for observation as there was spontaneous resolution of the hemorrhage.
Discussion: There is no widely available standard of care regarding endovascular management of pseudoaneurysms following a colostomy. Embolization was primarily performed in patients with hemorrhage, unstable hemodynamic status, and symptoms of intracranial mass effect. Surgery can be performed when embolization is unsuccessful or contraindicated such as local infection and distal ischemia. CT angiography is the standard method of evaluating GI bleeding in patients that have no bleeding source found on endoscopy, are hemodynamically stable, or are hemodynamically unstable while waiting for available angiography. Adjunct modalities for evaluating GI bleeds in post-surgical patients is crucial in select patients, as endoscopy is neither diagnostic nor therapeutic for pseudoaneurysm hemorrhage.
Disclosures:
Arjun Ponduri, MD, Elen Sarkisyan, DO, Scott Diamond, DO, Vishvinder Sharma, MD. P0773 - Peristomal Pseudoaneurysm Presenting as Blood in Colostomy Bag, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Valley Hospital Medical Center, Las Vegas, NV
Introduction: A pseudoaneurysm results from vascular injury and results in hemorrhage and adjacent hematoma. This is primarily the result of medical procedures such as angiograms and cardiac catheterizations but also often result from severe pancreatitis presenting as a GI bleed. Complications from pseudoaneurysms include rupture and hemorrhage. Rupture rates can be between 2-45% based on the location of the pseudoaneurysm. Mortality rates of hemorrhage range between 12.5-37%, with important risk factors including age and hypertension. We present a case of a patient who presented with frank blood in his colostomy bag from a hemorrhaging peristomal pseudoaneurysm.
Case Description/Methods: A 49 year old male had a history of severe, acute pancreatitis 17 months prior complicated by a colon perforation requiring an ex- lap with distal pancreatectomy and a left hemicolectomy with colostomy. He presented with bloody output in his colostomy bag. Patient also noted generalized abdominal pain around the colostomy bag.
Hemoglobin on admission was 12.1. A CT of the abdomen and pelvis with IV contrast showed peri- and intrapancreatic stranding suspicious for necrotizing pancreatitis with a pseudocyst extending from the pancreatic tail into iliopsoas muscle and dehiscence of the skin and subcutaneous tissue of lower ventral abdominal wall adjacent to his colostomy.
A CT angiography of the abdomen/pelvis was ordered revealing an 8 x 9 mm pseudoaneurysm within the open laparotomy external to the skin surface.
The patient’s hemoglobin dropped to 9.1 and IR attempted embolization; however it was too superficial. The surgical team opted for observation as there was spontaneous resolution of the hemorrhage.
Discussion: There is no widely available standard of care regarding endovascular management of pseudoaneurysms following a colostomy. Embolization was primarily performed in patients with hemorrhage, unstable hemodynamic status, and symptoms of intracranial mass effect. Surgery can be performed when embolization is unsuccessful or contraindicated such as local infection and distal ischemia. CT angiography is the standard method of evaluating GI bleeding in patients that have no bleeding source found on endoscopy, are hemodynamically stable, or are hemodynamically unstable while waiting for available angiography. Adjunct modalities for evaluating GI bleeds in post-surgical patients is crucial in select patients, as endoscopy is neither diagnostic nor therapeutic for pseudoaneurysm hemorrhage.
Disclosures:
Arjun Ponduri indicated no relevant financial relationships.
Elen Sarkisyan indicated no relevant financial relationships.
Scott Diamond indicated no relevant financial relationships.
Vishvinder Sharma indicated no relevant financial relationships.
Arjun Ponduri, MD, Elen Sarkisyan, DO, Scott Diamond, DO, Vishvinder Sharma, MD. P0773 - Peristomal Pseudoaneurysm Presenting as Blood in Colostomy Bag, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
