Sunday Poster Session
Category: GI Bleeding
P0782 - Atypical Hemolytic Uremic Syndrome (aHUS): An Initial Presentation of Helicobacter pylori
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Menna-Allah Elaskandrany, DO
Lenox Hill Hospital, Northwell Health, NY
Presenting Author(s)
Menna-Allah Elaskandrany, DO1, Mohamed Ismail, DO2, Jasmine Lee, DO3, Micheal Bebawy, DO2, Linda Kirschenbaum, DO1
1Lenox Hill Hospital, Northwell Health, New York, NY; 2Rutgers New Jersey Medical School, Newark, NJ; 3NYU Langone Health, New York, NY
Introduction: Atypical hemolytic uremic syndrome (aHUS) is a rare, rapidly progressive thrombotic microangiopathy (TMA) characterized by microangiopathic hemolytic anemia, acute kidney injury (AKI), and thrombocytopenia. While HUS is most commonly due to Shiga toxin producing E. coli, complement dysregulation can also lead to aHUS. Helicobacter pylori (H. pylori) has been rarely reported in the literature as a cause of TMA or aHUS. We present a case of aHUS as the initial presentation of an active H. pylori infection.
Case Description/Methods: A 61-year-old Filipino female with past medical history of hypertension and chronic kidney disease (CKD) stage 3 presented with lethargy, melena, and tachycardia with a hemoglobin of 6.3 g/dL. After receiving a blood transfusion, her tachycardia improved, but one hour later, she developed a fever of 101.4ºF with a HR of 145 bpm, concerning for acute transfusion reaction. She revealed history of Anti-Jra antibodies, and the reaction was attributed to these antibodies.
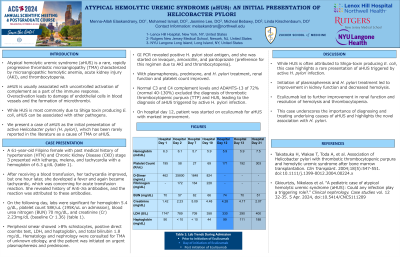
The following day, labs were significant for hemoglobin 5.4 g/dL, platelet count 58K/uL (195K/uL on admission), blood urea nitrogen (BUN) 70 mg/dL, and creatinine (Cr) 2.23mg/dL (baseline Cr 1.36). Peripheral smear showed >8% schistocytes, a positive direct coombs test, LDH, and haptoglobin, and total bilirubin 1.8 mg/dL. Hematology and nephrology were consulted for TMA of unknown etiology, and patient was initiated on urgent plasmapheresis and prednisone.
GI PCR revealed positive H. pylori stool antigen and she was started on levaquin, amoxicillin, and pantoprazole (preference for this regimen due to AKI and thrombocytopenia). With plasmapheresis, prednisone, and H. pylori treatment, renal function and platelet count improved. Normal C3 and C4 complement levels and ADAMTS-13 of 72% (normal 40-130%) excluded the diagnosis of thrombotic thrombocytopenic purpura (TTP) and HUS, leading to the diagnosis of aHUS triggered by active H. pylori infection. On hospital day 12, patient was started on eculizumab for aHUS with marked improvement.
Discussion: While HUS is often attributed to Shiga-toxin producing E. coli, this case highlights a rare presentation of aHUS triggered by active H. pylori infection. Initiation of plasmapheresis, H. pylori treatment, and eculizumab led to improvement in renal function and resolution of hemolysis and thrombocytopenia. This case underscores the importance of diagnosing and treating underlying causes of aHUS and highlights the novel association with H. pylori.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Menna-Allah Elaskandrany, DO1, Mohamed Ismail, DO2, Jasmine Lee, DO3, Micheal Bebawy, DO2, Linda Kirschenbaum, DO1. P0782 - Atypical Hemolytic Uremic Syndrome (aHUS): An Initial Presentation of <i>Helicobacter pylori</i>, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Lenox Hill Hospital, Northwell Health, New York, NY; 2Rutgers New Jersey Medical School, Newark, NJ; 3NYU Langone Health, New York, NY
Introduction: Atypical hemolytic uremic syndrome (aHUS) is a rare, rapidly progressive thrombotic microangiopathy (TMA) characterized by microangiopathic hemolytic anemia, acute kidney injury (AKI), and thrombocytopenia. While HUS is most commonly due to Shiga toxin producing E. coli, complement dysregulation can also lead to aHUS. Helicobacter pylori (H. pylori) has been rarely reported in the literature as a cause of TMA or aHUS. We present a case of aHUS as the initial presentation of an active H. pylori infection.
Case Description/Methods: A 61-year-old Filipino female with past medical history of hypertension and chronic kidney disease (CKD) stage 3 presented with lethargy, melena, and tachycardia with a hemoglobin of 6.3 g/dL. After receiving a blood transfusion, her tachycardia improved, but one hour later, she developed a fever of 101.4ºF with a HR of 145 bpm, concerning for acute transfusion reaction. She revealed history of Anti-Jra antibodies, and the reaction was attributed to these antibodies.
The following day, labs were significant for hemoglobin 5.4 g/dL, platelet count 58K/uL (195K/uL on admission), blood urea nitrogen (BUN) 70 mg/dL, and creatinine (Cr) 2.23mg/dL (baseline Cr 1.36). Peripheral smear showed >8% schistocytes, a positive direct coombs test, LDH, and haptoglobin, and total bilirubin 1.8 mg/dL. Hematology and nephrology were consulted for TMA of unknown etiology, and patient was initiated on urgent plasmapheresis and prednisone.
GI PCR revealed positive H. pylori stool antigen and she was started on levaquin, amoxicillin, and pantoprazole (preference for this regimen due to AKI and thrombocytopenia). With plasmapheresis, prednisone, and H. pylori treatment, renal function and platelet count improved. Normal C3 and C4 complement levels and ADAMTS-13 of 72% (normal 40-130%) excluded the diagnosis of thrombotic thrombocytopenic purpura (TTP) and HUS, leading to the diagnosis of aHUS triggered by active H. pylori infection. On hospital day 12, patient was started on eculizumab for aHUS with marked improvement.
Discussion: While HUS is often attributed to Shiga-toxin producing E. coli, this case highlights a rare presentation of aHUS triggered by active H. pylori infection. Initiation of plasmapheresis, H. pylori treatment, and eculizumab led to improvement in renal function and resolution of hemolysis and thrombocytopenia. This case underscores the importance of diagnosing and treating underlying causes of aHUS and highlights the novel association with H. pylori.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Menna-Allah Elaskandrany indicated no relevant financial relationships.
Mohamed Ismail indicated no relevant financial relationships.
Jasmine Lee indicated no relevant financial relationships.
Micheal Bebawy indicated no relevant financial relationships.
Linda Kirschenbaum indicated no relevant financial relationships.
Menna-Allah Elaskandrany, DO1, Mohamed Ismail, DO2, Jasmine Lee, DO3, Micheal Bebawy, DO2, Linda Kirschenbaum, DO1. P0782 - Atypical Hemolytic Uremic Syndrome (aHUS): An Initial Presentation of <i>Helicobacter pylori</i>, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
