Sunday Poster Session
Category: GI Bleeding
P0818 - Cystogastrostomy Complicated by Stent Erosion Into the Splenic Artery Causing Massive Upper Gastrointestinal Bleeding
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Bibek Saha, MD
Mayo Clinic
Rochester, MN
Presenting Author(s)
Bibek Saha, MD, Joelle Friesen, MD, Allison Reinhardt, MD, Victoria Kalinoski-Dubose, MD, Karthik Ravi, MD
Mayo Clinic, Rochester, MN
Introduction: Upper gastrointestinal bleeding (UGIB) is a frequent cause of hospitalizations with mortality rates between 2-15%. While common causes of massive UGIB are peptic ulcer disease, and esophageal varices, we present a rare case of splenic artery erosion by a stent in the setting of recent cystogastrostomy causing a brisk UGIB and hemorrhagic shock.
Case Description/Methods: A 75-year-old female with a history of non-metastatic pancreatic adenocarcinoma and pancreatitis with pseudocyst managed locally with endoscopic cystogastrostomy two months prior, was transferred to the ICU for hematemesis and melena complicated by hemorrhagic shock. She was admitted to the floor for somnolence after taking sedative medications for anxiety in anticipation of outpatient laparoscopic exploration for the pancreatic adenocarcinoma. On staging studies, she was found to have venous thromboembolism and was started on anticoagulation the day prior to the UGIB.
In the ICU, she was afebrile (36.5°C) tachycardic (118bpm), hypotensive (60/41mmHg), tachypneic (32breaths/min) with an oxygen saturation of 83%. On physical exam, she was obtunded with active hematemesis. Her abdomen was soft but distended at the left upper quadrant. Labs revealed a hemoglobin of 9.4 (11 the day prior) and leukocytosis (WBC= 42.4). ABG showed severe acidosis (pH=6.86), where lactate was 10.4. She was intubated, started on pressors and massive transfusion protocol. Computed Tomography (CT) angiogram of the abdomen and pelvis demonstrated splenic artery erosion by the stent associated with the cystogastrostomy with large active arterial extravasation into the stent which in turn decompressed into the stomach (Figure 1). Imaging also revealed splenic infarcts affecting >50% of spleen.
She underwent coil embolization of the splenic artery. After intervention, she improved hemodynamically and was extubated. However, there were concerns that the infarcted spleen and perisplenic fluid were infected prompting splenectomy, splenic abscess evacuation, stent removal and gastrostomy closure.
Discussion: Gastrointestinal bleeds are traditionally classified as an UGIB or lower GI bleed, where the former comprises approximately 75% of cases and is thought to be more severe. Cystogastrostomy is an effective endoscopic treatment for pancreatic pseudocysts with a low recurrence rate. However, splenic vascular injury should be in the differential diagnoses for patients with recent cystogastrostomy who present with massive UGIB.
Disclosures:
Bibek Saha, MD, Joelle Friesen, MD, Allison Reinhardt, MD, Victoria Kalinoski-Dubose, MD, Karthik Ravi, MD. P0818 - Cystogastrostomy Complicated by Stent Erosion Into the Splenic Artery Causing Massive Upper Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mayo Clinic, Rochester, MN
Introduction: Upper gastrointestinal bleeding (UGIB) is a frequent cause of hospitalizations with mortality rates between 2-15%. While common causes of massive UGIB are peptic ulcer disease, and esophageal varices, we present a rare case of splenic artery erosion by a stent in the setting of recent cystogastrostomy causing a brisk UGIB and hemorrhagic shock.
Case Description/Methods: A 75-year-old female with a history of non-metastatic pancreatic adenocarcinoma and pancreatitis with pseudocyst managed locally with endoscopic cystogastrostomy two months prior, was transferred to the ICU for hematemesis and melena complicated by hemorrhagic shock. She was admitted to the floor for somnolence after taking sedative medications for anxiety in anticipation of outpatient laparoscopic exploration for the pancreatic adenocarcinoma. On staging studies, she was found to have venous thromboembolism and was started on anticoagulation the day prior to the UGIB.
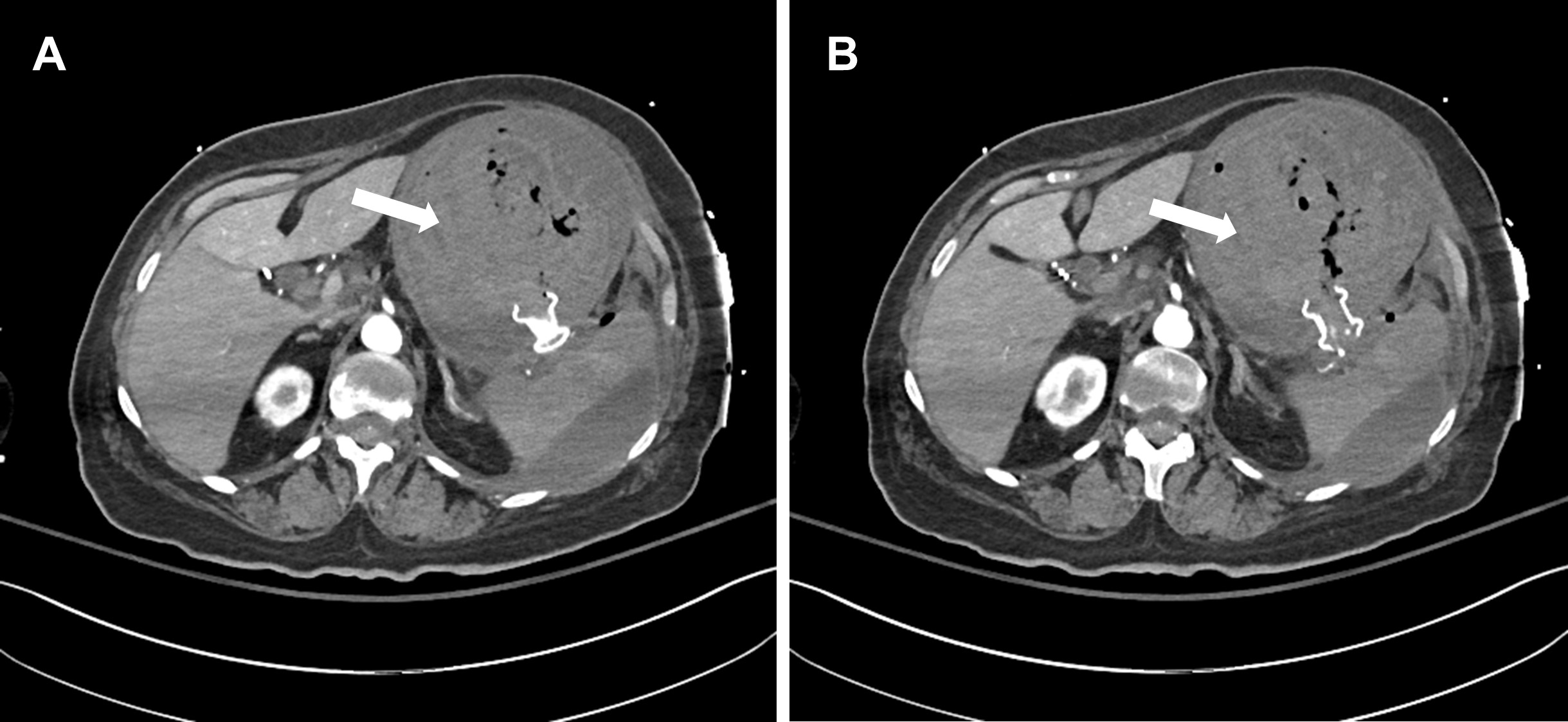
In the ICU, she was afebrile (36.5°C) tachycardic (118bpm), hypotensive (60/41mmHg), tachypneic (32breaths/min) with an oxygen saturation of 83%. On physical exam, she was obtunded with active hematemesis. Her abdomen was soft but distended at the left upper quadrant. Labs revealed a hemoglobin of 9.4 (11 the day prior) and leukocytosis (WBC= 42.4). ABG showed severe acidosis (pH=6.86), where lactate was 10.4. She was intubated, started on pressors and massive transfusion protocol. Computed Tomography (CT) angiogram of the abdomen and pelvis demonstrated splenic artery erosion by the stent associated with the cystogastrostomy with large active arterial extravasation into the stent which in turn decompressed into the stomach (Figure 1). Imaging also revealed splenic infarcts affecting >50% of spleen.
She underwent coil embolization of the splenic artery. After intervention, she improved hemodynamically and was extubated. However, there were concerns that the infarcted spleen and perisplenic fluid were infected prompting splenectomy, splenic abscess evacuation, stent removal and gastrostomy closure.
Discussion: Gastrointestinal bleeds are traditionally classified as an UGIB or lower GI bleed, where the former comprises approximately 75% of cases and is thought to be more severe. Cystogastrostomy is an effective endoscopic treatment for pancreatic pseudocysts with a low recurrence rate. However, splenic vascular injury should be in the differential diagnoses for patients with recent cystogastrostomy who present with massive UGIB.
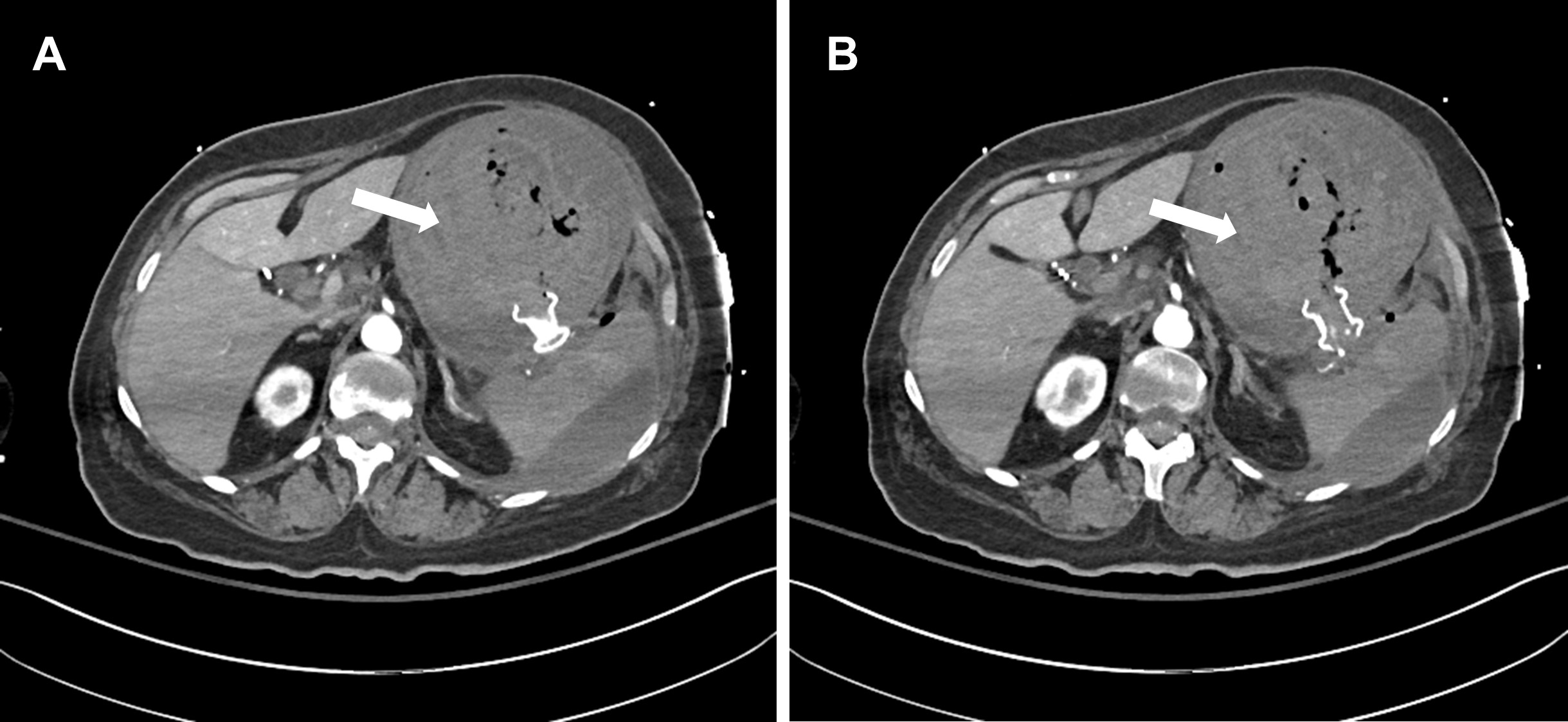
Figure: Figure 1. Computed Tomography angiogram of the abdomen and pelvis showing the splenic artery abutting the stent with artery erosion and active arterial extravasation (A) and bleeding into the stent (B) which is decompressing into a large blood-filled stomach (arrow).
Disclosures:
Bibek Saha indicated no relevant financial relationships.
Joelle Friesen indicated no relevant financial relationships.
Allison Reinhardt indicated no relevant financial relationships.
Victoria Kalinoski-Dubose indicated no relevant financial relationships.
Karthik Ravi indicated no relevant financial relationships.
Bibek Saha, MD, Joelle Friesen, MD, Allison Reinhardt, MD, Victoria Kalinoski-Dubose, MD, Karthik Ravi, MD. P0818 - Cystogastrostomy Complicated by Stent Erosion Into the Splenic Artery Causing Massive Upper Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
