Sunday Poster Session
Category: IBD
P0851 - The Urgency Numeric Rating Scale: Psychometric Evaluation in Adults With Crohn’s Disease
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Marla Dubinsky, MD
Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Marla C. Dubinsky, MD1, Aisha Vadhariya, 2, Sylvia Su, 2, Xian Zhou, 3, Frederick Durand, 2, Claudine Clucas, 4, Larissa Stassek, 4, Ariane Kawata, 4, Simon Travis, 5
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Eli Lilly and Company, Indianapolis, IN; 3Syneos Health, Morrisville, NC; 4Evidera, Bethesda, MD; 5University of Oxford, Oxford, England, United Kingdom
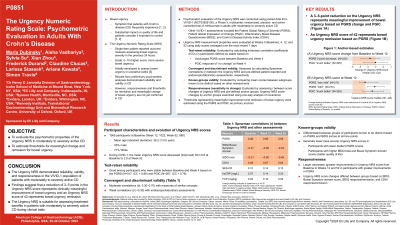
Introduction: Bowel urgency (BU) is a common symptom of Crohn’s disease (CD) that negatively impacts patients’ quality of life. The Urgency Numeric Rating Scale (NRS) is used to assess BU severity on an 11-point scale. This work evaluated the psychometric properties of the Urgency NRS in CD and estimated thresholds for meaningful change and remission for BU.
Methods: Pooled data from VIVID-1, a Phase 3, multicenter, randomized, placebo- and active-controlled study of mirikizumab in adults with moderately to severely active CD were analyzed. Reliability, validity, and responsiveness of the Urgency NRS were evaluated using average scores at Weeks (W)0, W4, W12, and 52. The Patient Global Rating of Severity (PGRS) and Patient Global Impression of Change (PGIC) were used as primary anchors to establish the Urgency NRS score thresholds for meaningful change and BU remission.
Results: The study included 1065 adults (mean age 36.2±13.0 years, 55% male, 71% White). The Urgency NRS weekly average score decreased from 6.6 at W0 to 2.9 at W52. Test-retest reliability was good for patients stable between W0 and W4, based on the PGRS (intraclass correlation coefficient [ICC] 0.86) and PGIC (ICC 0.78). At W12 and W52, the Urgency NRS showed moderate correlations (0.30 ≤ r < 0.70) with the PGRS and other related patient-reported outcome measures, demonstrating convergent validity. Correlations with endoscopic and laboratory assessments were weak (r < 0.30), demonstrating discriminant validity. The Urgency NRS could differentiate between distinct participant groups known to differ based on PGRS and Inflammatory Bowel Disease Questionnaire (IBDQ) Bowel Symptom domain scores. The Urgency NRS average score improvement from Baseline to W12 and W52 was statistically significantly different between most PGRS change and PGIC groups, as well as groups based on other assessments, indicating that the Urgency NRS could detect change. Anchor-based analysis showed that a 3–5-point reduction in the Urgency NRS score represented clinically meaningful improvement and an Urgency NRS score ≤2 represented BU remission.
Discussion: The results support the reliability, validity, responsiveness of the Urgency NRS and provide definitions of clinically meaningful improvement and BU remission in adults with moderately to severely active CD. The Urgency NRS can be considered suitable for assessing treatment benefits in CD.
Disclosures:
Marla C. Dubinsky, MD1, Aisha Vadhariya, 2, Sylvia Su, 2, Xian Zhou, 3, Frederick Durand, 2, Claudine Clucas, 4, Larissa Stassek, 4, Ariane Kawata, 4, Simon Travis, 5. P0851 - The Urgency Numeric Rating Scale: Psychometric Evaluation in Adults With Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Eli Lilly and Company, Indianapolis, IN; 3Syneos Health, Morrisville, NC; 4Evidera, Bethesda, MD; 5University of Oxford, Oxford, England, United Kingdom
Introduction: Bowel urgency (BU) is a common symptom of Crohn’s disease (CD) that negatively impacts patients’ quality of life. The Urgency Numeric Rating Scale (NRS) is used to assess BU severity on an 11-point scale. This work evaluated the psychometric properties of the Urgency NRS in CD and estimated thresholds for meaningful change and remission for BU.
Methods: Pooled data from VIVID-1, a Phase 3, multicenter, randomized, placebo- and active-controlled study of mirikizumab in adults with moderately to severely active CD were analyzed. Reliability, validity, and responsiveness of the Urgency NRS were evaluated using average scores at Weeks (W)0, W4, W12, and 52. The Patient Global Rating of Severity (PGRS) and Patient Global Impression of Change (PGIC) were used as primary anchors to establish the Urgency NRS score thresholds for meaningful change and BU remission.
Results: The study included 1065 adults (mean age 36.2±13.0 years, 55% male, 71% White). The Urgency NRS weekly average score decreased from 6.6 at W0 to 2.9 at W52. Test-retest reliability was good for patients stable between W0 and W4, based on the PGRS (intraclass correlation coefficient [ICC] 0.86) and PGIC (ICC 0.78). At W12 and W52, the Urgency NRS showed moderate correlations (0.30 ≤ r < 0.70) with the PGRS and other related patient-reported outcome measures, demonstrating convergent validity. Correlations with endoscopic and laboratory assessments were weak (r < 0.30), demonstrating discriminant validity. The Urgency NRS could differentiate between distinct participant groups known to differ based on PGRS and Inflammatory Bowel Disease Questionnaire (IBDQ) Bowel Symptom domain scores. The Urgency NRS average score improvement from Baseline to W12 and W52 was statistically significantly different between most PGRS change and PGIC groups, as well as groups based on other assessments, indicating that the Urgency NRS could detect change. Anchor-based analysis showed that a 3–5-point reduction in the Urgency NRS score represented clinically meaningful improvement and an Urgency NRS score ≤2 represented BU remission.
Discussion: The results support the reliability, validity, responsiveness of the Urgency NRS and provide definitions of clinically meaningful improvement and BU remission in adults with moderately to severely active CD. The Urgency NRS can be considered suitable for assessing treatment benefits in CD.
Disclosures:
Marla Dubinsky: AbbVie – Consultant. Abivax – Consultant. Arena – Consultant. AstraZeneca – Consultant. Bristol Myers Squibb – Consultant. Celgene – Consultant. Eli Lilly – Consultant. Genentech – Consultant. Gilead – Consultant. Janssen – Consultant. Pfizer Inc – Consultant. Prometheus Labs – Consultant. Takeda – Consultant.
Aisha Vadhariya: Eli Lilly and Company – Employee, Stock Options.
Sylvia Su: Eli Lilly and Company – Employee, Stock Options.
Xian Zhou: Syneos Health – Employee.
Frederick Durand: Eli Lilly and Company – Employee, Stock Options.
Claudine Clucas: Evidera – Employee.
Larissa Stassek: Evidera – Employee.
Ariane Kawata: Evidera – Employee.
Simon Travis: AbbVie – Grant/Research Support. Buhlmann – Grant/Research Support. ECCO – Grant/Research Support. Eli Lilly and Company – Grant/Research Support. Ferring Pharmaceuticals – Grant/Research Support. International Organization for the Study of IBD – Grant/Research Support. Janssen – Grant/Research Support. MSD – Grant/Research Support. Normal Collision Foundation – Grant/Research Support. Pfizer – Grant/Research Support. Procter & Gamble – Grant/Research Support. Schering-Plough – Grant/Research Support. Takeda – Grant/Research Support. UCB – Grant/Research Support. Vifor Pharma – Grant/Research Support. Warner Chilcott – Grant/Research Support.
Marla C. Dubinsky, MD1, Aisha Vadhariya, 2, Sylvia Su, 2, Xian Zhou, 3, Frederick Durand, 2, Claudine Clucas, 4, Larissa Stassek, 4, Ariane Kawata, 4, Simon Travis, 5. P0851 - The Urgency Numeric Rating Scale: Psychometric Evaluation in Adults With Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
