Sunday Poster Session
Category: IBD
P0857 - Osteoporosis Screening: Utilization Trends in High-Dose Steroids for Crohn’s Disease and Ulcerative Colitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- JS
Jessica Sosio, DO
Indiana University School of Medicine
Evansville, IN
Presenting Author(s)
Jessica Sosio, DO1, Karla Geisse, DO, MPH1, Marcos A. Alberto, MD1, Lindsey Valdiviez, DO1, Adrian Singson, MD2, Oluwagbenga Serrano, MD, FACG3
1Indiana University School of Medicine, Evansville, IN; 2Indiana University School of Medicine, Vincennes, IN; 3Good Samaritan Hospital, Vincennes, IN
Introduction: Osteoporosis (OP) is a common complication of inflammatory bowel disease (IBD), and affects up to 42% of patients. OP is usually the result of steroid use and malabsorption leading to calcium and vitamin D deficiencies. This typically occurs more in Crohn’s disease (CD), and is particularly seen with significant steroid use (SSU) ( >7.5 mg/day of prednisone-equivalent for longer than 3 consecutive months). A 2019 meta-analysis found that IBD patients have a 32% increased risk of developing osteoporotic fractures, which is associated with significant morbidity, mortality, and healthcare cost. Gastroenterology professional societies recommend regular OP screening in IBD, especially with SSU. However, studies show low screening rates and adherence to guidelines. We conducted a retrospective chart review on OP screening utilization in patients with SSU in the IBD population within our rural gastroenterology clinic.
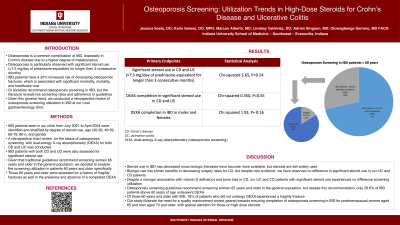
Methods: IBD patients seen in our clinic from July 2021 to April 2024 were identified and stratified by degree of steroid use, age, and gender. A retrospective review was conducted for ulcerative colitis (UC) and CD on the status of their OP screening with dual-energy X-ray absorptiometry (DEXA) in the presence of SSU. The primary outcomes were steroid use and DEXA completion. Chi-squared testing was performed with a 95% confidence interval (CI).
Results: We identified 100 patients, 45 UC and 55 CD. There was no statistical difference in SSU (Chi-squared 3.65, P=0.54) and SSU DEXA completion (Chi-squared 0.35, P=0.55) between UC and CD. There was no statistical difference in IBD DEXA completion between genders (Chi-squared 1.93, P= 0.16). However, only 28.6% of IBD patients above 60 years of age underwent DEXA. 16% of IBD patients who did not undergo DEXA experienced a fracture.
Discussion: Steroid use in IBD has decreased since biologic therapies became more available, and biologic use has shown benefits in decreasing surgery rates for CD. Despite new evidence, we have observed no difference in SSU in our UC and CD patients. Additionally, even with a stronger association to vitamin D deficiency and bone loss in CD, our UC and CD patients with SSU experienced no difference in OP screening utilization. Only 28.6% of IBD patients above 60 years of age underwent DEXA, which also suggests a deviation from traditional guidelines recommending screening women 65 years and older in the general population.
Disclosures:
Jessica Sosio, DO1, Karla Geisse, DO, MPH1, Marcos A. Alberto, MD1, Lindsey Valdiviez, DO1, Adrian Singson, MD2, Oluwagbenga Serrano, MD, FACG3. P0857 - Osteoporosis Screening: Utilization Trends in High-Dose Steroids for Crohn’s Disease and Ulcerative Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Indiana University School of Medicine, Evansville, IN; 2Indiana University School of Medicine, Vincennes, IN; 3Good Samaritan Hospital, Vincennes, IN
Introduction: Osteoporosis (OP) is a common complication of inflammatory bowel disease (IBD), and affects up to 42% of patients. OP is usually the result of steroid use and malabsorption leading to calcium and vitamin D deficiencies. This typically occurs more in Crohn’s disease (CD), and is particularly seen with significant steroid use (SSU) ( >7.5 mg/day of prednisone-equivalent for longer than 3 consecutive months). A 2019 meta-analysis found that IBD patients have a 32% increased risk of developing osteoporotic fractures, which is associated with significant morbidity, mortality, and healthcare cost. Gastroenterology professional societies recommend regular OP screening in IBD, especially with SSU. However, studies show low screening rates and adherence to guidelines. We conducted a retrospective chart review on OP screening utilization in patients with SSU in the IBD population within our rural gastroenterology clinic.
Methods: IBD patients seen in our clinic from July 2021 to April 2024 were identified and stratified by degree of steroid use, age, and gender. A retrospective review was conducted for ulcerative colitis (UC) and CD on the status of their OP screening with dual-energy X-ray absorptiometry (DEXA) in the presence of SSU. The primary outcomes were steroid use and DEXA completion. Chi-squared testing was performed with a 95% confidence interval (CI).
Results: We identified 100 patients, 45 UC and 55 CD. There was no statistical difference in SSU (Chi-squared 3.65, P=0.54) and SSU DEXA completion (Chi-squared 0.35, P=0.55) between UC and CD. There was no statistical difference in IBD DEXA completion between genders (Chi-squared 1.93, P= 0.16). However, only 28.6% of IBD patients above 60 years of age underwent DEXA. 16% of IBD patients who did not undergo DEXA experienced a fracture.
Discussion: Steroid use in IBD has decreased since biologic therapies became more available, and biologic use has shown benefits in decreasing surgery rates for CD. Despite new evidence, we have observed no difference in SSU in our UC and CD patients. Additionally, even with a stronger association to vitamin D deficiency and bone loss in CD, our UC and CD patients with SSU experienced no difference in OP screening utilization. Only 28.6% of IBD patients above 60 years of age underwent DEXA, which also suggests a deviation from traditional guidelines recommending screening women 65 years and older in the general population.
Disclosures:
Jessica Sosio indicated no relevant financial relationships.
Karla Geisse indicated no relevant financial relationships.
Marcos Alberto indicated no relevant financial relationships.
Lindsey Valdiviez indicated no relevant financial relationships.
Adrian Singson indicated no relevant financial relationships.
Oluwagbenga Serrano: MERCK – Stock-publicly held company(excluding mutual/index funds).
Jessica Sosio, DO1, Karla Geisse, DO, MPH1, Marcos A. Alberto, MD1, Lindsey Valdiviez, DO1, Adrian Singson, MD2, Oluwagbenga Serrano, MD, FACG3. P0857 - Osteoporosis Screening: Utilization Trends in High-Dose Steroids for Crohn’s Disease and Ulcerative Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
