Sunday Poster Session
Category: IBD
P0863 - Comparing the Risk of Venous Thromboembolism and Pulmonary Embolism in Inflammatory Bowel Disease Patients Treated With Different Biologics: A Propensity Score-Matched, Retrospective Cohort Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- FA
Feyzullah Aksan, MD
Renaissance School of Medicine, Stony Brook University
Port Jefferson Station, NY
Presenting Author(s)
Feyzullah Aksan, MD1, Farah Monzur, MD, FACG2
1Renaissance School of Medicine, Stony Brook University, Port Jefferson Station, NY; 2Renaissance School of Medicine at Stony Brook University, Stony Brook, NY
Introduction: Patients with inflammatory bowel disease (IBD) have a 2-3 times higher risk of venous thromboembolic events (VTE) compared to non-IBD controls. The pathogenesis of VTE in IBD is complex, with chronic inflammation playing a pivotal role. VTE in IBD is characterized by high recurrence rates and poor prognosis, with a mortality rate about 2.5 times higher than IBD patients without VTE. Currently, no studies compare VTE risk in IBD patients treated with different biologics. This study aims to address this gap.
Methods: We conducted a retrospective cohort study using TriNetX, a multi-institutional database, to compare VTE risk in IBD patients treated with different biologics. Patients aged ≥18 with Crohn’s Disease (CD) or Ulcerative Colitis (UC) between January 1, 2016, and April 18, 2023, were split into three cohorts based on biologic class: anti-TNFs, anti-integrin (VDZ), and interleukin 12/23 inhibitors (UST) . Each cohort was separately compared. We utilized 1:1 propensity score matching (PSM) for demographics, age, gender, comorbidities, IBD subtypes, concurrent medications, hypercoagulability states, hormones (steroids, OCPs, estrogen, androgen), and anticoagulants. Clinical outcomes within 1 year of biologic initiation, including VTE (upper or lower extremity DVT) and PE, were assessed. HR and 95% CI were used for risk assessment, with α < 0.05 for significance.
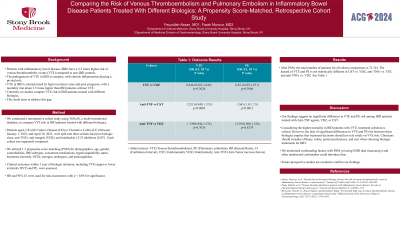
Results: After PSM, the total number of patients for all cohort comparisons is 72,744. The hazard of VTE and PE is not statistically different in UST vs. VDZ, anti-TNFs vs. UST, and anti-TNFs vs. VDZ. See Table 1.
Discussion: Our findings suggest no significant difference in VTE and PE risk among IBD patients treated with Anti-TNF agents, VDZ, or UST. Considering the higher mortality in IBD patients with VTE, treatment selection is critical. However, the lack of significant differences in VTE and PE risk between these biologics implies that treatment decisions should not rely solely on VTE risk. Clinicians should consider efficacy, safety, patient preferences, and cost when choosing biologic treatments for IBD. We minimized confounding factors with PSM yet using EMR data (inaccuracy) and other undetected confounders could introduce bias. Future prospective studies are needed to confirm our findings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Feyzullah Aksan, MD1, Farah Monzur, MD, FACG2. P0863 - Comparing the Risk of Venous Thromboembolism and Pulmonary Embolism in Inflammatory Bowel Disease Patients Treated With Different Biologics: A Propensity Score-Matched, Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Renaissance School of Medicine, Stony Brook University, Port Jefferson Station, NY; 2Renaissance School of Medicine at Stony Brook University, Stony Brook, NY
Introduction: Patients with inflammatory bowel disease (IBD) have a 2-3 times higher risk of venous thromboembolic events (VTE) compared to non-IBD controls. The pathogenesis of VTE in IBD is complex, with chronic inflammation playing a pivotal role. VTE in IBD is characterized by high recurrence rates and poor prognosis, with a mortality rate about 2.5 times higher than IBD patients without VTE. Currently, no studies compare VTE risk in IBD patients treated with different biologics. This study aims to address this gap.
Methods: We conducted a retrospective cohort study using TriNetX, a multi-institutional database, to compare VTE risk in IBD patients treated with different biologics. Patients aged ≥18 with Crohn’s Disease (CD) or Ulcerative Colitis (UC) between January 1, 2016, and April 18, 2023, were split into three cohorts based on biologic class: anti-TNFs, anti-integrin (VDZ), and interleukin 12/23 inhibitors (UST) . Each cohort was separately compared. We utilized 1:1 propensity score matching (PSM) for demographics, age, gender, comorbidities, IBD subtypes, concurrent medications, hypercoagulability states, hormones (steroids, OCPs, estrogen, androgen), and anticoagulants. Clinical outcomes within 1 year of biologic initiation, including VTE (upper or lower extremity DVT) and PE, were assessed. HR and 95% CI were used for risk assessment, with α < 0.05 for significance.
Results: After PSM, the total number of patients for all cohort comparisons is 72,744. The hazard of VTE and PE is not statistically different in UST vs. VDZ, anti-TNFs vs. UST, and anti-TNFs vs. VDZ. See Table 1.
Discussion: Our findings suggest no significant difference in VTE and PE risk among IBD patients treated with Anti-TNF agents, VDZ, or UST. Considering the higher mortality in IBD patients with VTE, treatment selection is critical. However, the lack of significant differences in VTE and PE risk between these biologics implies that treatment decisions should not rely solely on VTE risk. Clinicians should consider efficacy, safety, patient preferences, and cost when choosing biologic treatments for IBD. We minimized confounding factors with PSM yet using EMR data (inaccuracy) and other undetected confounders could introduce bias. Future prospective studies are needed to confirm our findings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Feyzullah Aksan indicated no relevant financial relationships.
Farah Monzur: Gather-Ed – Consultant, Speakers Bureau. Medtronic (Covidien) – Consultant. Prometheus – Consultant.
Feyzullah Aksan, MD1, Farah Monzur, MD, FACG2. P0863 - Comparing the Risk of Venous Thromboembolism and Pulmonary Embolism in Inflammatory Bowel Disease Patients Treated With Different Biologics: A Propensity Score-Matched, Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

