Sunday Poster Session
Category: IBD
P0901 - Changed Opioid Prescribing Practices for Inflammatory Bowel Disease After the Opioid Epidemic Declaration: A Retrospective Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- KS
Katherine Shepherd, MD
West Virginia University
Morgantown, WV
Presenting Author(s)
Katherine Shepherd, MD, Alyssa Lorenze, MD, Momin Khan, MD, Jennifer Hadam-Veverka, MD, Swapna Gayam, MD
West Virginia University, Morgantown, WV
Introduction: Patients with inflammatory bowel disease (IBD) commonly suffer from relapsing and remitting abdominal pain even in the presence of clinical remission, and opioids are often prescribed despite known risks. In October 2017, the United States Department of Health and Human Services declared a public health emergency, the opioid epidemic. The Appalachian region, notoriously characterized by economic hardship and low access to care has been identified as an opioid epidemic “hot spot.” We aim to characterize opioid use in patients with IBD and determine if prescriber practices have changed after the declaration of public health crisis in newly established IBD patients at a large academic institution in the heart of Appalachia.
Methods: We conducted a retrospective cohort study of patients with Crohn’s Disease (CD) or Ulcerative Colitis (UC) establishing care at the outpatient West Virginia University Gastroenterology Clinic from 2015 to 2019. Patients were divided into two groups, those presenting prior to the declaration of the opioid epidemic from 2015-2017 and those presenting after from 2017-2019, with October 26, 2017 being the transition point. Statistical analysis was used to determine if the declaration of a public health emergency had an impact on opioid prescriber practice and patient opioid use.
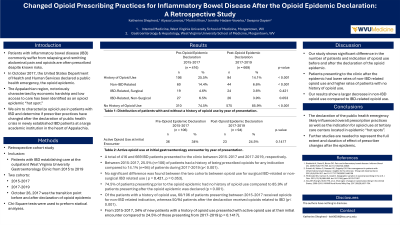
Results: A total of 416 and 669 IBD patients presented to the clinic between 2015-2017 and 2017-2019, respectively. Between 2015-2017, 25.4% (n=106) of patients had a history of being prescribed opioids for any indication compared to 16.3% (n=94) of patients during 2017-2019 (p< 0.001). Of the patients with a history of opioid use, a majority of patients presenting between 2015-2017 received opioids for non-IBD related indication, whereas the majority of patients after the declaration received opioids related to IBD (p< 0.001). Inpatient opioid prescriptions and opioids prescribed at discharge were increased in CD patients compared to UC patients (p< 0.01). In addition, there was a statistically significant decrease in hydrocodone prescriptions after the declaration of the public health emergency (p< 0.05).
Discussion: Our study shows significant difference in the number of patients presenting to the gastroenterology clinic with a history of being prescribed opioids before and after the declaration of the opioid epidemic. Therefore, the declaration of the public health emergency likely contributed to overall prescription practice as well as the indication in which opioids were prescribed.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Katherine Shepherd, MD, Alyssa Lorenze, MD, Momin Khan, MD, Jennifer Hadam-Veverka, MD, Swapna Gayam, MD. P0901 - Changed Opioid Prescribing Practices for Inflammatory Bowel Disease After the Opioid Epidemic Declaration: A Retrospective Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
West Virginia University, Morgantown, WV
Introduction: Patients with inflammatory bowel disease (IBD) commonly suffer from relapsing and remitting abdominal pain even in the presence of clinical remission, and opioids are often prescribed despite known risks. In October 2017, the United States Department of Health and Human Services declared a public health emergency, the opioid epidemic. The Appalachian region, notoriously characterized by economic hardship and low access to care has been identified as an opioid epidemic “hot spot.” We aim to characterize opioid use in patients with IBD and determine if prescriber practices have changed after the declaration of public health crisis in newly established IBD patients at a large academic institution in the heart of Appalachia.
Methods: We conducted a retrospective cohort study of patients with Crohn’s Disease (CD) or Ulcerative Colitis (UC) establishing care at the outpatient West Virginia University Gastroenterology Clinic from 2015 to 2019. Patients were divided into two groups, those presenting prior to the declaration of the opioid epidemic from 2015-2017 and those presenting after from 2017-2019, with October 26, 2017 being the transition point. Statistical analysis was used to determine if the declaration of a public health emergency had an impact on opioid prescriber practice and patient opioid use.
Results: A total of 416 and 669 IBD patients presented to the clinic between 2015-2017 and 2017-2019, respectively. Between 2015-2017, 25.4% (n=106) of patients had a history of being prescribed opioids for any indication compared to 16.3% (n=94) of patients during 2017-2019 (p< 0.001). Of the patients with a history of opioid use, a majority of patients presenting between 2015-2017 received opioids for non-IBD related indication, whereas the majority of patients after the declaration received opioids related to IBD (p< 0.001). Inpatient opioid prescriptions and opioids prescribed at discharge were increased in CD patients compared to UC patients (p< 0.01). In addition, there was a statistically significant decrease in hydrocodone prescriptions after the declaration of the public health emergency (p< 0.05).
Discussion: Our study shows significant difference in the number of patients presenting to the gastroenterology clinic with a history of being prescribed opioids before and after the declaration of the opioid epidemic. Therefore, the declaration of the public health emergency likely contributed to overall prescription practice as well as the indication in which opioids were prescribed.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Katherine Shepherd indicated no relevant financial relationships.
Alyssa Lorenze indicated no relevant financial relationships.
Momin Khan indicated no relevant financial relationships.
Jennifer Hadam-Veverka: Abbive – Speakers Bureau. Bristol-Myers Squibb – Speakers Bureau. Janssen – Speakers Bureau. Takeda – Speakers Bureau.
Swapna Gayam indicated no relevant financial relationships.
Katherine Shepherd, MD, Alyssa Lorenze, MD, Momin Khan, MD, Jennifer Hadam-Veverka, MD, Swapna Gayam, MD. P0901 - Changed Opioid Prescribing Practices for Inflammatory Bowel Disease After the Opioid Epidemic Declaration: A Retrospective Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
