Sunday Poster Session
Category: IBD
P0902 - Prevalence and Current Management of Inflammatory Bowel Disease in West Virginia
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- KS
Katherine Shepherd, MD
West Virginia University
Morgantown, WV
Presenting Author(s)
Katherine Shepherd, MD, Ethan M.. Cohen, MD, Taylor B. Kenneda, MD, VM Rajendran, PhD, Murugesan Velayutham, PhD, Jennifer Hadam-Veverka, MD, Justin T.. Kupec, MD
West Virginia University, Morgantown, WV
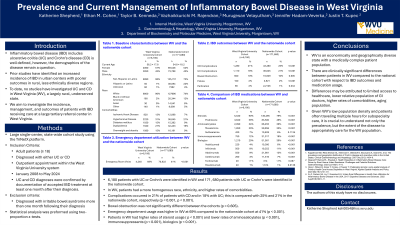
Introduction: Inflammatory bowel disease (IBD), which includes ulcerative colitis (UC) and Crohn’s disease (CD), is well defined, but demographics of the disease remain a question. Prior studies have identified an increased incidence of IBD in urban centers with poorer outcomes in rural, less ethnically diverse regions. To date, no studies have investigated UC and CD in West Virginia (WV), a rural, medically underserved state. We aim to investigate the incidence, management, and outcomes of patients with IBD receiving care at a large tertiary referral center in WV.
Methods: We conducted a large, single-center, state-wide cohort study using the TriNetX platform. Adult patients (≥ 18 years old) diagnosed with either UC or CD who had an outpatient appointment within the West Virginia University. UC and CD diagnoses were confirmed by documentation of accepted IBD treatment (e.g. corticosteroids, aminosalicylates, immunosuppressants, or biologics) at least one month after their diagnosis. Patients were excluded if they were diagnosed with irritable bowel syndrome more than one month following their diagnosis. To identify a national cohort, identical inclusion and exclusion criteria were used to within TriNetX. Statistical analysis was preformed using two-proportion z-tests.
Results: A total of 6180 patients with UC or Crohn’s were identified in WV with an average age of 56.9 ± 17.6. 95.4% of patients were white (n=5900) followed by 2.3% Black or African American (n=140). In WV, 47% of the patients were diagnosed with CD, and 53% were diagnosed with UC. Complications occurred in 21% of patients with CD and in 18% with UC; this is compared with 25% and 21% in the nationwide cohort, respectively (p< 0.001). Bowel obstruction was the most diagnosed complication in both the WV and nationwide cohort, representing 10% the identified population (p=0.60). Corticosteroid use was 90% and 79%, respectively (p< 0.001). Biologic treatment was 20% in WV compared to 30% nationwide (p< 0.001).
Discussion: West Virginia is an economically and geographically diverse state with a medically complex patient population. Given its low population density with patients often traveling multiple hours for subspecialty care, it is crucial to understand not only the prevalence of IBD in WV, but the extent of the disease to appropriately care for the population and improve outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Katherine Shepherd, MD, Ethan M.. Cohen, MD, Taylor B. Kenneda, MD, VM Rajendran, PhD, Murugesan Velayutham, PhD, Jennifer Hadam-Veverka, MD, Justin T.. Kupec, MD. P0902 - Prevalence and Current Management of Inflammatory Bowel Disease in West Virginia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
West Virginia University, Morgantown, WV
Introduction: Inflammatory bowel disease (IBD), which includes ulcerative colitis (UC) and Crohn’s disease (CD), is well defined, but demographics of the disease remain a question. Prior studies have identified an increased incidence of IBD in urban centers with poorer outcomes in rural, less ethnically diverse regions. To date, no studies have investigated UC and CD in West Virginia (WV), a rural, medically underserved state. We aim to investigate the incidence, management, and outcomes of patients with IBD receiving care at a large tertiary referral center in WV.
Methods: We conducted a large, single-center, state-wide cohort study using the TriNetX platform. Adult patients (≥ 18 years old) diagnosed with either UC or CD who had an outpatient appointment within the West Virginia University. UC and CD diagnoses were confirmed by documentation of accepted IBD treatment (e.g. corticosteroids, aminosalicylates, immunosuppressants, or biologics) at least one month after their diagnosis. Patients were excluded if they were diagnosed with irritable bowel syndrome more than one month following their diagnosis. To identify a national cohort, identical inclusion and exclusion criteria were used to within TriNetX. Statistical analysis was preformed using two-proportion z-tests.
Results: A total of 6180 patients with UC or Crohn’s were identified in WV with an average age of 56.9 ± 17.6. 95.4% of patients were white (n=5900) followed by 2.3% Black or African American (n=140). In WV, 47% of the patients were diagnosed with CD, and 53% were diagnosed with UC. Complications occurred in 21% of patients with CD and in 18% with UC; this is compared with 25% and 21% in the nationwide cohort, respectively (p< 0.001). Bowel obstruction was the most diagnosed complication in both the WV and nationwide cohort, representing 10% the identified population (p=0.60). Corticosteroid use was 90% and 79%, respectively (p< 0.001). Biologic treatment was 20% in WV compared to 30% nationwide (p< 0.001).
Discussion: West Virginia is an economically and geographically diverse state with a medically complex patient population. Given its low population density with patients often traveling multiple hours for subspecialty care, it is crucial to understand not only the prevalence of IBD in WV, but the extent of the disease to appropriately care for the population and improve outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Katherine Shepherd indicated no relevant financial relationships.
Ethan Cohen indicated no relevant financial relationships.
Taylor Kenneda indicated no relevant financial relationships.
VM Rajendran indicated no relevant financial relationships.
Murugesan Velayutham indicated no relevant financial relationships.
Jennifer Hadam-Veverka: Abbive – Speakers Bureau. Bristol-Myers Squibb – Speakers Bureau. Janssen – Speakers Bureau. Takeda – Speakers Bureau.
Justin Kupec indicated no relevant financial relationships.
Katherine Shepherd, MD, Ethan M.. Cohen, MD, Taylor B. Kenneda, MD, VM Rajendran, PhD, Murugesan Velayutham, PhD, Jennifer Hadam-Veverka, MD, Justin T.. Kupec, MD. P0902 - Prevalence and Current Management of Inflammatory Bowel Disease in West Virginia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
