Sunday Poster Session
Category: IBD
P0930 - Gastrointestinal Infection Prior to Immune Checkpoint Inhibition Hinders Treatment Efficacy and Increases the Risk for Checkpoint-Inhibitor Colitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- KA
Kian Abdul-Baki, DO
University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Malek Shatila, MD1, Kian Abdul-Baki, DO2, Andres Rivera, MD3, Kei Takigawa, MD3, Irene J. Lee, MD3, Andrew Sullivan, MD4, Tanvi Gupta, MD5, Linfeng Lu, MD3, Raakhi Menon, DO2, Ayesha Khan, DO2, Hamza Salim, MD2, Elliot Axel. Baerman, MD3, Carolina Colli Cruz, MD6, Cristina M. Natha, MD5, Varun Vemulapalli, MD5, Garrett T. Coleman, 7, Krishnavathana Varatharajalu, MD1, Yan Zhou, MD8, Hao Chi Zhang, MD6, Mehnaz A. Shafi, MD8, Yinghong Wang, MD, PhD8
1The University of Texas MD Anderson Cancer Center, Houston, TX; 2University of Texas Medical Branch, Galveston, TX; 3Baylor College of Medicine, Houston, TX; 4University of Texas Health Science Center, Houston, TX; 5University of Texas Health, McGovern Medical School, Houston, TX; 6MD Anderson Cancer Center, Houston, TX; 7University of Texas Medical Branch, John Sealy School of Medicine, Galveston, TX; 8University of Texas MD Anderson Cancer Center, Houston, TX
Introduction: The gut microbiome has received increasing attention in recent years for its role in cancer responsiveness to treatment and treatment-related toxicities. Gastrointestinal (GI) infections often arise due to and cause intestinal dysbiosis, which can impact immune checkpoint inhibitor (ICI) efficacy and increase the risk of adverse effects such as colitis. Our study aims to explore the impact of GI infection prior to ICI initiation on the incidence and severity of immune-mediated colitis (IMC) as well as on patient survival.
Methods: This was a single center, retrospective review including all patients who received ICIs between 01/2010 to 02/2024 and developed IMC. Patients were screened for IMC based on stool tests, then divided into two groups depending on their history of GI infection within three months prior to ICI initiation. We collected patient demographic, and IMC and GI infection-related clinical data.
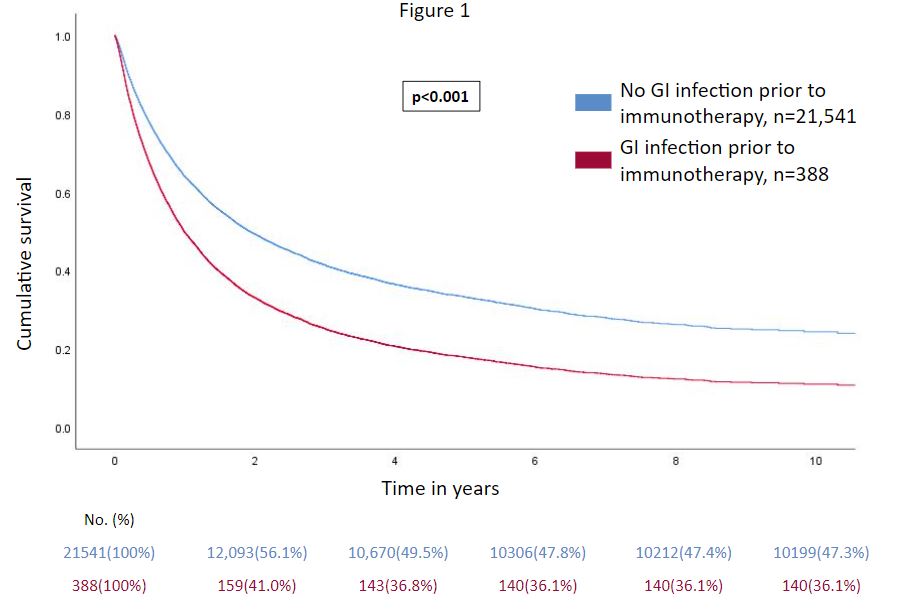
Results: 1,132 patients met the study criteria and were included, 34 of whom had a history of GI infection prior to ICI. GI infections were most commonly caused by Clostridiodes difficile and treated with oral antibiotics for a median of 10 days (IQR: 7-14 days). The incidence of IMC was increased within this subgroup, with 8.7% (34/393) of patients with prior GI infection developing colitis compared to 5.1% (1098/21,736) of those without (p=0.002). IMC symptoms and severity were similar between both groups, as were outcomes such as hospitalization, symptom resolution, and recurrence rates (p >0.05). Treatments used in both groups did not differ significantly, with the exception of fecal microbiota transplantation (FMT), which was used more in the prior infection group (p=0.029). Outcomes of FMT-treated patients with or without prior GI infection did not differ significantly (p >0.05). Finally, on multivariate Cox survival analysis, prior GI infection was independently associated with mortality (OR: 1.6, CI:1.4-1.8; p< 0.001) among ICI-treated patients after controlling for age, sex, and race.
Discussion: Our study is the first to explore the impact of GI infection prior to ICI initiation on IMC risk and patient survival. GI infection may interfere with ICI efficacy as reflected by worse overall survival among these patients and may increase the risk of developing IMC. These findings may be due to the association of GI infection with dysbiosis of the gut microbiome. Further studies with a larger study group are needed to validate these results.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Malek Shatila, MD1, Kian Abdul-Baki, DO2, Andres Rivera, MD3, Kei Takigawa, MD3, Irene J. Lee, MD3, Andrew Sullivan, MD4, Tanvi Gupta, MD5, Linfeng Lu, MD3, Raakhi Menon, DO2, Ayesha Khan, DO2, Hamza Salim, MD2, Elliot Axel. Baerman, MD3, Carolina Colli Cruz, MD6, Cristina M. Natha, MD5, Varun Vemulapalli, MD5, Garrett T. Coleman, 7, Krishnavathana Varatharajalu, MD1, Yan Zhou, MD8, Hao Chi Zhang, MD6, Mehnaz A. Shafi, MD8, Yinghong Wang, MD, PhD8. P0930 - Gastrointestinal Infection Prior to Immune Checkpoint Inhibition Hinders Treatment Efficacy and Increases the Risk for Checkpoint-Inhibitor Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The University of Texas MD Anderson Cancer Center, Houston, TX; 2University of Texas Medical Branch, Galveston, TX; 3Baylor College of Medicine, Houston, TX; 4University of Texas Health Science Center, Houston, TX; 5University of Texas Health, McGovern Medical School, Houston, TX; 6MD Anderson Cancer Center, Houston, TX; 7University of Texas Medical Branch, John Sealy School of Medicine, Galveston, TX; 8University of Texas MD Anderson Cancer Center, Houston, TX
Introduction: The gut microbiome has received increasing attention in recent years for its role in cancer responsiveness to treatment and treatment-related toxicities. Gastrointestinal (GI) infections often arise due to and cause intestinal dysbiosis, which can impact immune checkpoint inhibitor (ICI) efficacy and increase the risk of adverse effects such as colitis. Our study aims to explore the impact of GI infection prior to ICI initiation on the incidence and severity of immune-mediated colitis (IMC) as well as on patient survival.
Methods: This was a single center, retrospective review including all patients who received ICIs between 01/2010 to 02/2024 and developed IMC. Patients were screened for IMC based on stool tests, then divided into two groups depending on their history of GI infection within three months prior to ICI initiation. We collected patient demographic, and IMC and GI infection-related clinical data.
Results: 1,132 patients met the study criteria and were included, 34 of whom had a history of GI infection prior to ICI. GI infections were most commonly caused by Clostridiodes difficile and treated with oral antibiotics for a median of 10 days (IQR: 7-14 days). The incidence of IMC was increased within this subgroup, with 8.7% (34/393) of patients with prior GI infection developing colitis compared to 5.1% (1098/21,736) of those without (p=0.002). IMC symptoms and severity were similar between both groups, as were outcomes such as hospitalization, symptom resolution, and recurrence rates (p >0.05). Treatments used in both groups did not differ significantly, with the exception of fecal microbiota transplantation (FMT), which was used more in the prior infection group (p=0.029). Outcomes of FMT-treated patients with or without prior GI infection did not differ significantly (p >0.05). Finally, on multivariate Cox survival analysis, prior GI infection was independently associated with mortality (OR: 1.6, CI:1.4-1.8; p< 0.001) among ICI-treated patients after controlling for age, sex, and race.
Discussion: Our study is the first to explore the impact of GI infection prior to ICI initiation on IMC risk and patient survival. GI infection may interfere with ICI efficacy as reflected by worse overall survival among these patients and may increase the risk of developing IMC. These findings may be due to the association of GI infection with dysbiosis of the gut microbiome. Further studies with a larger study group are needed to validate these results.
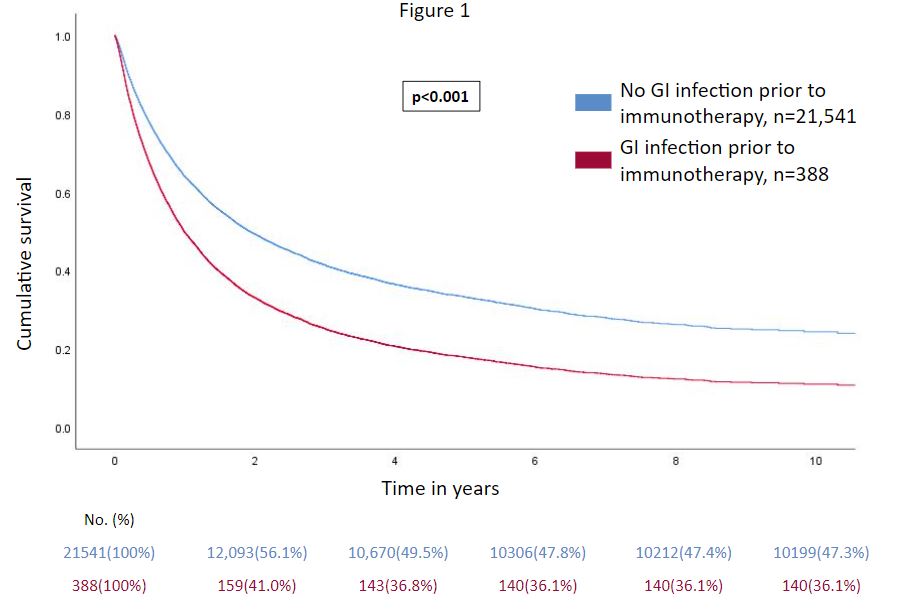
Figure: Figure 1. Cox Hazard survival curve for patients receiving immune checkpoint inhibitors who did or did not develop a gastrointestinal infection prior to treatment initiation
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Malek Shatila indicated no relevant financial relationships.
Kian Abdul-Baki indicated no relevant financial relationships.
Andres Rivera indicated no relevant financial relationships.
Kei Takigawa indicated no relevant financial relationships.
Irene Lee indicated no relevant financial relationships.
Andrew Sullivan indicated no relevant financial relationships.
Tanvi Gupta indicated no relevant financial relationships.
Linfeng Lu indicated no relevant financial relationships.
Raakhi Menon indicated no relevant financial relationships.
Ayesha Khan indicated no relevant financial relationships.
Hamza Salim indicated no relevant financial relationships.
Elliot Baerman indicated no relevant financial relationships.
Carolina Colli Cruz indicated no relevant financial relationships.
Cristina Natha indicated no relevant financial relationships.
Varun Vemulapalli indicated no relevant financial relationships.
Garrett Coleman indicated no relevant financial relationships.
Krishnavathana Varatharajalu indicated no relevant financial relationships.
Yan Zhou indicated no relevant financial relationships.
Hao Chi Zhang indicated no relevant financial relationships.
Mehnaz Shafi indicated no relevant financial relationships.
Yinghong Wang: AzurRx – Consultant. Ilyapharma – Consultant. IOTA – Consultant. Sorriso – Consultant. Tillotts – Consultant.
Malek Shatila, MD1, Kian Abdul-Baki, DO2, Andres Rivera, MD3, Kei Takigawa, MD3, Irene J. Lee, MD3, Andrew Sullivan, MD4, Tanvi Gupta, MD5, Linfeng Lu, MD3, Raakhi Menon, DO2, Ayesha Khan, DO2, Hamza Salim, MD2, Elliot Axel. Baerman, MD3, Carolina Colli Cruz, MD6, Cristina M. Natha, MD5, Varun Vemulapalli, MD5, Garrett T. Coleman, 7, Krishnavathana Varatharajalu, MD1, Yan Zhou, MD8, Hao Chi Zhang, MD6, Mehnaz A. Shafi, MD8, Yinghong Wang, MD, PhD8. P0930 - Gastrointestinal Infection Prior to Immune Checkpoint Inhibition Hinders Treatment Efficacy and Increases the Risk for Checkpoint-Inhibitor Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
