Sunday Poster Session
Category: IBD
P0937 - Optimizing Nutrition Education in a Dedicated Inflammatory Bowel Diseases Clinic
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Thomas W. Fredrick, MD
Mayo Clinic
Rochester, MN
Presenting Author(s)
Thomas W. Fredrick, MD, June Tome, MD, Camille Kezer, MD, Sunanda V. Kane, MD, MSPH
Mayo Clinic, Rochester, MN
Introduction: Patients with inflammatory bowel disease (IBD) frequently ask their providers for nutritional or dietary recommendations, however providers are limited in both time and knowledge to adequately address their questions. In this single-center study we sought to improve provider experiences with nutrition counseling for patients seen in a dedicated IBD clinic.
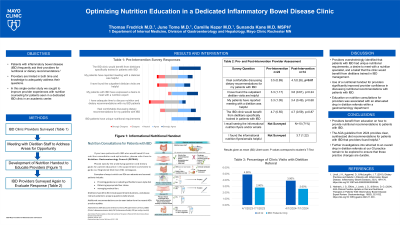
Methods: To understand the current state, providers including gastroenterology fellows, attendings, and advanced practice providers were surveyed (Table 1). Responses were graded on either yes/no or with a 5-point Likert scale. Following the pre-intervention survey, we discussed with registered dieticians how to address key concerns and developed an informational handout (Figure 1) based upon current guidelines for nutritional management in IBD. Handouts were displayed in clinical workspaces for both providers and patients to view. After the study period of 5 weeks, providers were surveyed again to evaluate their experience with nutritional management of patients with IBD post-intervention. Changes in survey responses were analyzed using Student’s T-test.
Results: 22 providers completed the pre-intervention survey. 100% of respondents in the pre-intervention survey either agreed (n=12) or strongly agreed (n=10) that IBD patients have unique nutritional requirements, and 72% (16/22) strongly agreed that the clinic would benefit from more access to dieticians 41% of providers either strongly disagreed (1/22) or disagreed (8/22) that they had enough time to address nutritional concerns, and 50% either were neutral (8/22) or disagreed (3/22) that they felt comfortable discussing nutritional recommendations with IBD patients. 14 providers completed the post-intervention survey, with 70% (10/14) of respondents viewing the handouts and 57% (8/14) reporting that they found the handouts helpful. A significant number of providers reported improvement in their comfort level discussing nutrition and dietary recommendations with IBD patients, with mean Likert score increasing from 3.5 to 4.1 (p=0.01).
Discussion: In this quality improvement study, we identified key issues that prevented providers from addressing patient desire for nutritional counseling. By collaborating with registered dieticians, we developed informational handouts to help providers address key nutritional issues. This intervention significantly improved provider confidence.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Thomas W. Fredrick, MD, June Tome, MD, Camille Kezer, MD, Sunanda V. Kane, MD, MSPH. P0937 - Optimizing Nutrition Education in a Dedicated Inflammatory Bowel Diseases Clinic, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mayo Clinic, Rochester, MN
Introduction: Patients with inflammatory bowel disease (IBD) frequently ask their providers for nutritional or dietary recommendations, however providers are limited in both time and knowledge to adequately address their questions. In this single-center study we sought to improve provider experiences with nutrition counseling for patients seen in a dedicated IBD clinic.
Methods: To understand the current state, providers including gastroenterology fellows, attendings, and advanced practice providers were surveyed (Table 1). Responses were graded on either yes/no or with a 5-point Likert scale. Following the pre-intervention survey, we discussed with registered dieticians how to address key concerns and developed an informational handout (Figure 1) based upon current guidelines for nutritional management in IBD. Handouts were displayed in clinical workspaces for both providers and patients to view. After the study period of 5 weeks, providers were surveyed again to evaluate their experience with nutritional management of patients with IBD post-intervention. Changes in survey responses were analyzed using Student’s T-test.
Results: 22 providers completed the pre-intervention survey. 100% of respondents in the pre-intervention survey either agreed (n=12) or strongly agreed (n=10) that IBD patients have unique nutritional requirements, and 72% (16/22) strongly agreed that the clinic would benefit from more access to dieticians 41% of providers either strongly disagreed (1/22) or disagreed (8/22) that they had enough time to address nutritional concerns, and 50% either were neutral (8/22) or disagreed (3/22) that they felt comfortable discussing nutritional recommendations with IBD patients. 14 providers completed the post-intervention survey, with 70% (10/14) of respondents viewing the handouts and 57% (8/14) reporting that they found the handouts helpful. A significant number of providers reported improvement in their comfort level discussing nutrition and dietary recommendations with IBD patients, with mean Likert score increasing from 3.5 to 4.1 (p=0.01).
Discussion: In this quality improvement study, we identified key issues that prevented providers from addressing patient desire for nutritional counseling. By collaborating with registered dieticians, we developed informational handouts to help providers address key nutritional issues. This intervention significantly improved provider confidence.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Thomas Fredrick indicated no relevant financial relationships.
June Tome indicated no relevant financial relationships.
Camille Kezer indicated no relevant financial relationships.
Sunanda Kane: Janssen – Advisory Committee/Board Member.
Thomas W. Fredrick, MD, June Tome, MD, Camille Kezer, MD, Sunanda V. Kane, MD, MSPH. P0937 - Optimizing Nutrition Education in a Dedicated Inflammatory Bowel Diseases Clinic, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
