Sunday Poster Session
Category: IBD
P0939 - Factors Associated With 30-Day Hospital Readmission in Pediatric Patients With Inflammatory Bowel Disease: A Multicenter Retrospective Cohort Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Nadaa Kemmou, MD
Johns Hopkins All Children's Hospital
St. Petersburg, FL
Presenting Author(s)
Nadaa Kemmou, MD1, Racha Khalaf, MD2, Kristen Calhoun, MD1, Jamie Fierstein, PhD1, John Morrison, MD, PhD1
1Johns Hopkins All Children's Hospital, St. Petersburg, FL; 2University of South Florida, Tampa, FL
Introduction: Hospitalizations are increasing for children with Inflammatory Bowel Disease (IBD) in the U.S., and pediatric patients with IBD are at increased risk of readmission relative to their adult counterparts. The primary objective of this study is to identify patient and hospitalization factors associated with 30-day all-cause hospital readmission among pediatric patients with IBD.
Methods: We performed a multicenter retrospective cohort study using the Pediatric Health Information System® (PHIS) database. De-identified data from 49 freestanding children’s hospitals were obtained on patients ages 0-21 years with an APR-DRG for IBD between 1/1/2018 and 12/31/2022. Our primary outcome was defined as readmission for any reason within 30 days of discharge from a hospitalization for treatment of IBD. Demographic factors and medical care received during index admission were extracted from PHIS. Multivariable mixed effects logistic regression was used to evaluate associations between our primary outcome and predictors of interest while accounting for clustering of patients within hospitals.
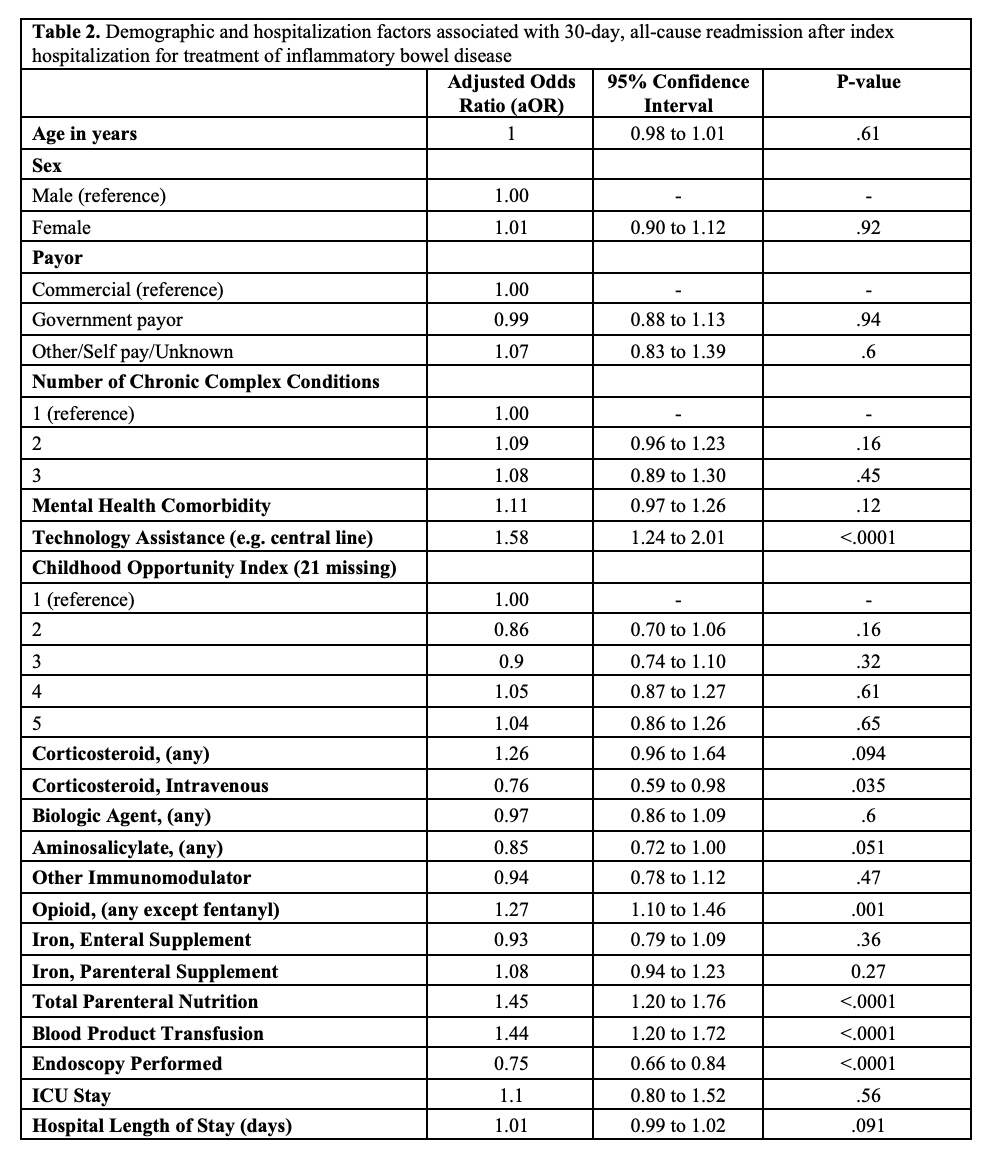
Results: Among 10,119 patients admitted for management of IBD, 1,525 (15%) were readmitted within 30 days of discharge. Rates of readmission ranged from 11-24% across all sites. The median (IQR) age of patients was 14.9 (11.8, 17) years; 43.4% had 2 or more chronic complex conditions and 23.5% had a comorbid mental health condition. Sixty-nine percent of patients received IV corticosteroids, 49.1% a biologic immunomodulatory agent, 9.8% total parenteral nutrition (TPN), and 10.3% blood products during hospitalization. Multivariable regression estimates are displayed in Table 2. Technology assistance (aOR 1.58, 95% CI 1.24-2.01), receipt of opioids (aOR 1.27, 95% CI 1.10-1.46), receipt of TPN (aOR 1.45, 95% CI 1.200-1.76), and transfusion of blood products (aOR 1.44, 95% CI 1.20-1.72) were associated with greater odds of readmission. Conversely, patients who received IV corticosteroids (aOR 0.76, 95% CI 0.59-0.98) or underwent an endoscopy (aOR 0.75, 95% CI 0.66-0.84) had lower odds of readmission.
Discussion: The number of pediatric patients with IBD who are readmitted within 30 days is significant. Within this study population, we identified multiple patient factors and interventions associated with readmission which may be used to inform targeted efforts to improve patient outcomes. Further investigation is required to understand why certain factors are associated with increased or decreased risk of readmission.
Disclosures:
Nadaa Kemmou, MD1, Racha Khalaf, MD2, Kristen Calhoun, MD1, Jamie Fierstein, PhD1, John Morrison, MD, PhD1. P0939 - Factors Associated With 30-Day Hospital Readmission in Pediatric Patients With Inflammatory Bowel Disease: A Multicenter Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Johns Hopkins All Children's Hospital, St. Petersburg, FL; 2University of South Florida, Tampa, FL
Introduction: Hospitalizations are increasing for children with Inflammatory Bowel Disease (IBD) in the U.S., and pediatric patients with IBD are at increased risk of readmission relative to their adult counterparts. The primary objective of this study is to identify patient and hospitalization factors associated with 30-day all-cause hospital readmission among pediatric patients with IBD.
Methods: We performed a multicenter retrospective cohort study using the Pediatric Health Information System® (PHIS) database. De-identified data from 49 freestanding children’s hospitals were obtained on patients ages 0-21 years with an APR-DRG for IBD between 1/1/2018 and 12/31/2022. Our primary outcome was defined as readmission for any reason within 30 days of discharge from a hospitalization for treatment of IBD. Demographic factors and medical care received during index admission were extracted from PHIS. Multivariable mixed effects logistic regression was used to evaluate associations between our primary outcome and predictors of interest while accounting for clustering of patients within hospitals.
Results: Among 10,119 patients admitted for management of IBD, 1,525 (15%) were readmitted within 30 days of discharge. Rates of readmission ranged from 11-24% across all sites. The median (IQR) age of patients was 14.9 (11.8, 17) years; 43.4% had 2 or more chronic complex conditions and 23.5% had a comorbid mental health condition. Sixty-nine percent of patients received IV corticosteroids, 49.1% a biologic immunomodulatory agent, 9.8% total parenteral nutrition (TPN), and 10.3% blood products during hospitalization. Multivariable regression estimates are displayed in Table 2. Technology assistance (aOR 1.58, 95% CI 1.24-2.01), receipt of opioids (aOR 1.27, 95% CI 1.10-1.46), receipt of TPN (aOR 1.45, 95% CI 1.200-1.76), and transfusion of blood products (aOR 1.44, 95% CI 1.20-1.72) were associated with greater odds of readmission. Conversely, patients who received IV corticosteroids (aOR 0.76, 95% CI 0.59-0.98) or underwent an endoscopy (aOR 0.75, 95% CI 0.66-0.84) had lower odds of readmission.
Discussion: The number of pediatric patients with IBD who are readmitted within 30 days is significant. Within this study population, we identified multiple patient factors and interventions associated with readmission which may be used to inform targeted efforts to improve patient outcomes. Further investigation is required to understand why certain factors are associated with increased or decreased risk of readmission.
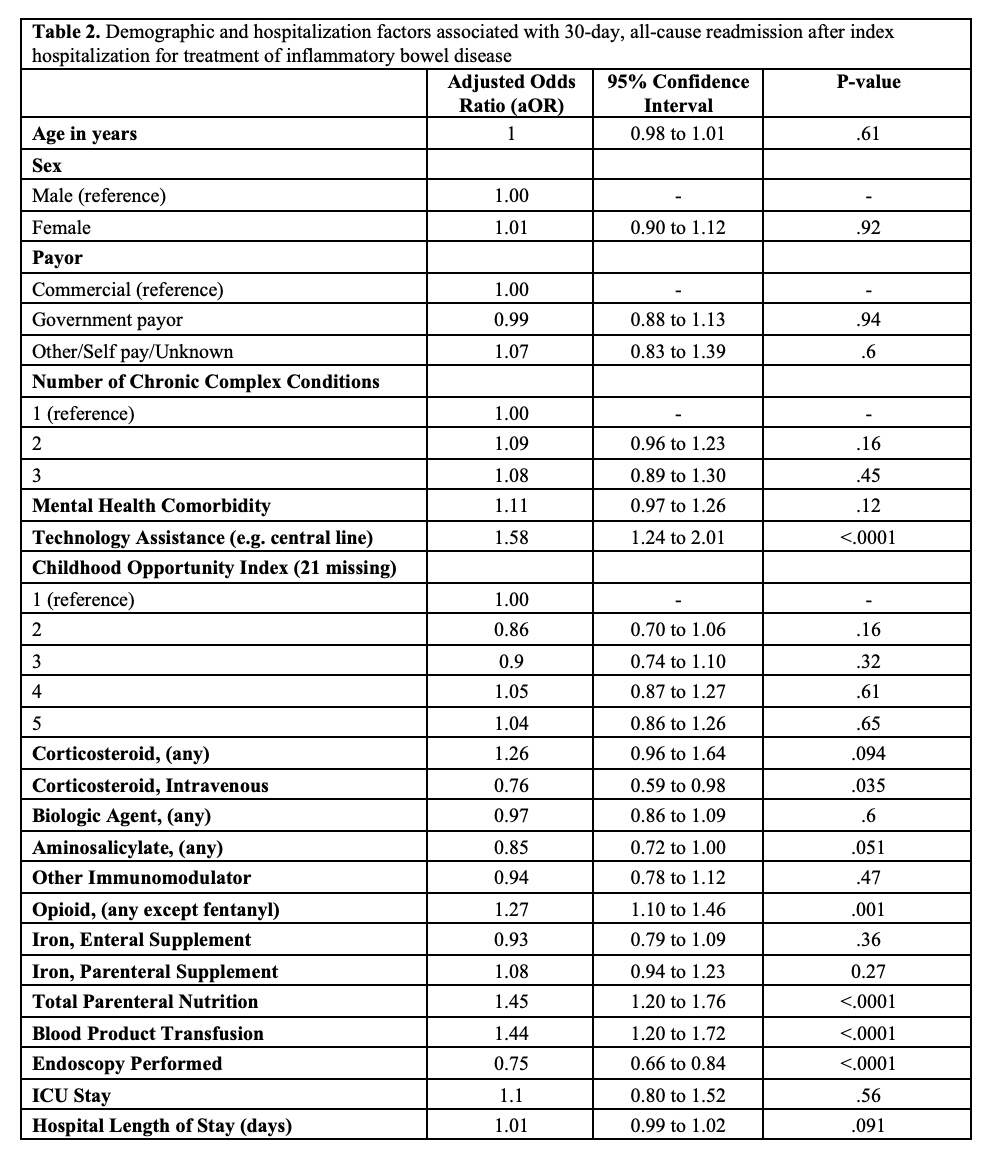
Figure: Table 2
Disclosures:
Nadaa Kemmou indicated no relevant financial relationships.
Racha Khalaf indicated no relevant financial relationships.
Kristen Calhoun indicated no relevant financial relationships.
Jamie Fierstein indicated no relevant financial relationships.
John Morrison indicated no relevant financial relationships.
Nadaa Kemmou, MD1, Racha Khalaf, MD2, Kristen Calhoun, MD1, Jamie Fierstein, PhD1, John Morrison, MD, PhD1. P0939 - Factors Associated With 30-Day Hospital Readmission in Pediatric Patients With Inflammatory Bowel Disease: A Multicenter Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
