Sunday Poster Session
Category: IBD
P0964 - IBD and Major Depression: Associated with Age, Sex, Smoking, Severity, and Extra-Intestinal Manifestations
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- SP
Sanket Patel, DO
Virtua Health System
Voorhees, NJ
Presenting Author(s)
Award: Presidential Poster Award
Sanket Patel, DO1, Philip Debbas, PhD2, Sweta Sinha, PhD2, Shaohong Yang, MD2, Jenna Holmes, 2, Colleen Gwarnicki, 3, Andres Yarur, MD4, Phillip Gu, MD2, Eric Vasiliauskas, MD2, David Ziring, MD4, Shervin Rabizadeh, MD, MBA2, Stephan Targan, MD2, Gil Y. Melmed, MD4, Talin Haritunians, MD2, Edward Feldman, MD2, Dalin Li, PhD4, Dermot McGovern, MD, PhD2
1Virtua Health System, Voorhees, NJ; 2Inflammatory Bowel Disease Center, Cedars-Sinai Medical Center, Los Angeles, CA; 3Cedars-Sinai Medical Center, Playa Vista, CA; 4Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Approximately 25% of Inflammatory Bowel Disease (IBD) patients experience depression, complicating clinical management. The bidirectional interplay between depression and IBD is poorly understood. It is unclear whether IBD triggers depression due to stress or if inflammation directly impacts mood regulation. Despite advancements in screening, gaps remain in understanding the clinical, genetic, and serologic characteristics of IBD patients with depression.
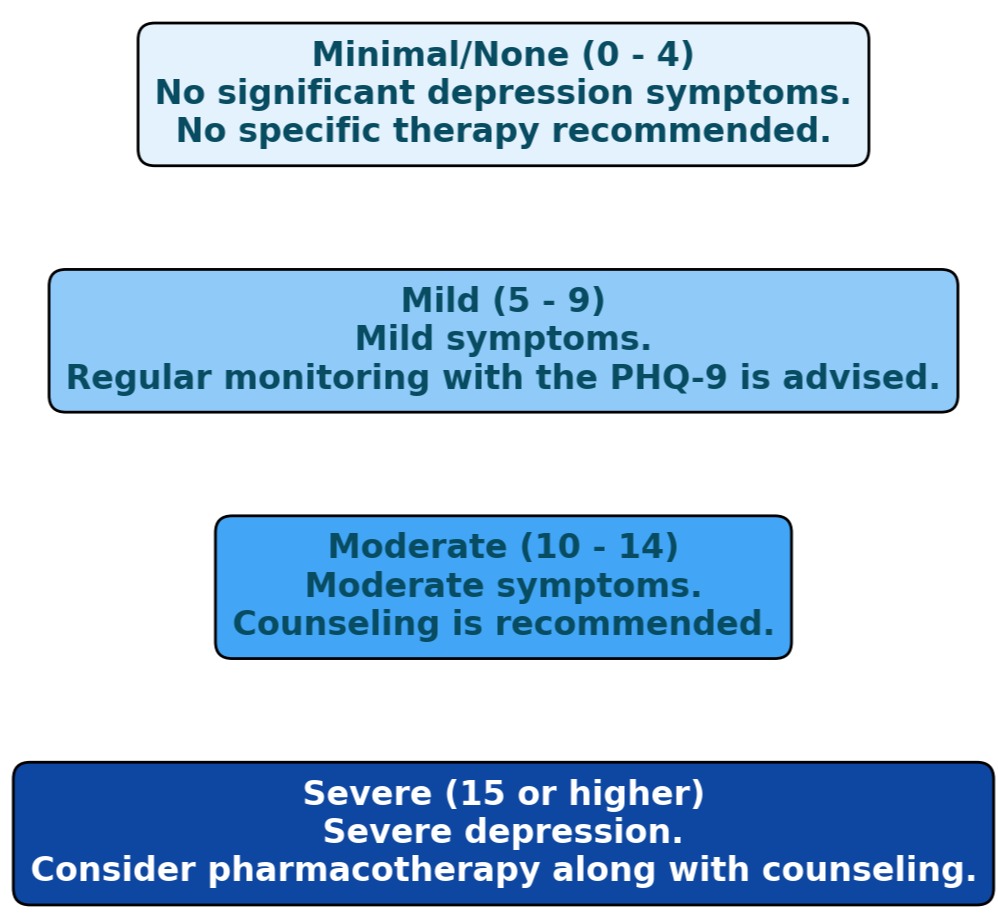
Methods: We analyzed electronic health record data from the MIRIAD Biobank, including Patient Health Questionnaire (PHQ-2 and PHQ-9) scores, ICD-9 and ICD-10 codes, and anti-depressant prescriptions linked to diagnosis codes for IBD patients. Out of 1795 patients, depression scores of 3, 2, 1, and 0 were assigned to severe (major), moderate, mild, or no depression, respectively (Figure 1). Generalized linear model, with adjustment for demographics including age and sex when appropriate, was utilized to determine the association between major depression and clinical phenotypes to mitigate confounding factors. Genotypes were generated using Immunochip, and IBD-related serologies were measured via ELISA. All participants provided informed consent and the study was IRB-approved.
Results: Among 1795 IBD patients with depression data, 49.2% had an episode of major depression, 10.2% had moderate or mild depression, and 40.6% had minimal or no depression. Age, females, smoking status, CD over UC, and CD location (ileocolonic vs colonic) were significantly associated with high depression score and major depression versus no depression in people with IBD (table 1). The presence of any extra-intestinal manifestations (EIMs) was significantly associated with major depression (table 1). The association between smoking status, female sex, & EIMs and major depression was consistent in both UC and CD cohorts (table 1). After correction for multiple testing, no significant association between depression and IBD-associated serology or genetic variant (including polygenic risk scores) were observed.
Discussion: This study underscores a significant prevalence of major depression in IBD influenced by clinical and demographic factors. The association between depression and smoking in both CD and UC despite tobacco exposure’s discordant effect on disease course in UC/CD is notable. More work to determine cause and effect phenomena with smoking and the relationship between depression and surgery, disease activity and associated genetic variants are in progress.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sanket Patel, DO1, Philip Debbas, PhD2, Sweta Sinha, PhD2, Shaohong Yang, MD2, Jenna Holmes, 2, Colleen Gwarnicki, 3, Andres Yarur, MD4, Phillip Gu, MD2, Eric Vasiliauskas, MD2, David Ziring, MD4, Shervin Rabizadeh, MD, MBA2, Stephan Targan, MD2, Gil Y. Melmed, MD4, Talin Haritunians, MD2, Edward Feldman, MD2, Dalin Li, PhD4, Dermot McGovern, MD, PhD2. P0964 - IBD and Major Depression: Associated with Age, Sex, Smoking, Severity, and Extra-Intestinal Manifestations, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Sanket Patel, DO1, Philip Debbas, PhD2, Sweta Sinha, PhD2, Shaohong Yang, MD2, Jenna Holmes, 2, Colleen Gwarnicki, 3, Andres Yarur, MD4, Phillip Gu, MD2, Eric Vasiliauskas, MD2, David Ziring, MD4, Shervin Rabizadeh, MD, MBA2, Stephan Targan, MD2, Gil Y. Melmed, MD4, Talin Haritunians, MD2, Edward Feldman, MD2, Dalin Li, PhD4, Dermot McGovern, MD, PhD2
1Virtua Health System, Voorhees, NJ; 2Inflammatory Bowel Disease Center, Cedars-Sinai Medical Center, Los Angeles, CA; 3Cedars-Sinai Medical Center, Playa Vista, CA; 4Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Approximately 25% of Inflammatory Bowel Disease (IBD) patients experience depression, complicating clinical management. The bidirectional interplay between depression and IBD is poorly understood. It is unclear whether IBD triggers depression due to stress or if inflammation directly impacts mood regulation. Despite advancements in screening, gaps remain in understanding the clinical, genetic, and serologic characteristics of IBD patients with depression.
Methods: We analyzed electronic health record data from the MIRIAD Biobank, including Patient Health Questionnaire (PHQ-2 and PHQ-9) scores, ICD-9 and ICD-10 codes, and anti-depressant prescriptions linked to diagnosis codes for IBD patients. Out of 1795 patients, depression scores of 3, 2, 1, and 0 were assigned to severe (major), moderate, mild, or no depression, respectively (Figure 1). Generalized linear model, with adjustment for demographics including age and sex when appropriate, was utilized to determine the association between major depression and clinical phenotypes to mitigate confounding factors. Genotypes were generated using Immunochip, and IBD-related serologies were measured via ELISA. All participants provided informed consent and the study was IRB-approved.
Results: Among 1795 IBD patients with depression data, 49.2% had an episode of major depression, 10.2% had moderate or mild depression, and 40.6% had minimal or no depression. Age, females, smoking status, CD over UC, and CD location (ileocolonic vs colonic) were significantly associated with high depression score and major depression versus no depression in people with IBD (table 1). The presence of any extra-intestinal manifestations (EIMs) was significantly associated with major depression (table 1). The association between smoking status, female sex, & EIMs and major depression was consistent in both UC and CD cohorts (table 1). After correction for multiple testing, no significant association between depression and IBD-associated serology or genetic variant (including polygenic risk scores) were observed.
Discussion: This study underscores a significant prevalence of major depression in IBD influenced by clinical and demographic factors. The association between depression and smoking in both CD and UC despite tobacco exposure’s discordant effect on disease course in UC/CD is notable. More work to determine cause and effect phenomena with smoking and the relationship between depression and surgery, disease activity and associated genetic variants are in progress.
Figure: PHQ9 Interpretation Figure 1
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sanket Patel: Abbvie – Speakers Bureau. BMS – Speakers Bureau. Eli Lilly – Speakers Bureau. Pfizer – Speakers Bureau. Takeda – Speakers Bureau.
Philip Debbas indicated no relevant financial relationships.
Sweta Sinha indicated no relevant financial relationships.
Shaohong Yang indicated no relevant financial relationships.
Jenna Holmes indicated no relevant financial relationships.
Colleen Gwarnicki indicated no relevant financial relationships.
Andres Yarur: AbbVie – Consultant, served on clinical trial steering committee. Abivax – Advisory Committee/Board Member, Consultant. Arena – Consultant, served on clinical trial steering committee. Boehringer Ingelheim – Advisory Committee/Board Member, Consultant. Bristol Myers Squibb – Consultant, served on clinical trial steering committee. Celltrion – Consultant, served on clinical trial steering committee. Johnson and Johnson – Advisory Committee/Board Member, Consultant. Pfizer – Consultant, served on clinical trial steering committee. Takeda – Consultant, served on clinical trial steering committee.
Phillip Gu: Abbvie – Consultant.
Eric Vasiliauskas indicated no relevant financial relationships.
David Ziring: Abbvie Pharmaceuticals – Speakers Bureau. Prometheus Laboratories – Speakers Bureau. Regeneron – Speakers Bureau.
Shervin Rabizadeh: Janssen – Advisor or Review Panel Member. Pfizer – Advisor or Review Panel Member. Prometheus – Advisor or Review Panel Member.
Stephan Targan indicated no relevant financial relationships.
Gil Y. Melmed: AbbVie – Consultant. Arena Biopharmaceuticals – Consultant. Boehringer-Ingelheim – Consultant. Bristol Myers Squibb-Celgene – Consultant. Dieta – Consultant. Eli Lilly – Consultant. Ferring – Consultant. Fresenius Kabi – Consultant. Genentech – Consultant. Gilead – Consultant. Janssen Immunology – Consultant. Oshi Health – Consultant. Pfizer – Consultant, Grant/Research Support. Prometheus Labs – Consultant. Samsung Bioepis – Consultant. Shionogi – Consultant. Takeda – Consultant. Techlab – Consultant. Viatris – Consultant.
Talin Haritunians indicated no relevant financial relationships.
Edward Feldman indicated no relevant financial relationships.
Dalin Li indicated no relevant financial relationships.
Dermot McGovern: Merck – Consultant. Prometheus Biosciences – Consultant, Stock Options. Prometheus Laboratories – Consultant. Takeda – Consultant.
Sanket Patel, DO1, Philip Debbas, PhD2, Sweta Sinha, PhD2, Shaohong Yang, MD2, Jenna Holmes, 2, Colleen Gwarnicki, 3, Andres Yarur, MD4, Phillip Gu, MD2, Eric Vasiliauskas, MD2, David Ziring, MD4, Shervin Rabizadeh, MD, MBA2, Stephan Targan, MD2, Gil Y. Melmed, MD4, Talin Haritunians, MD2, Edward Feldman, MD2, Dalin Li, PhD4, Dermot McGovern, MD, PhD2. P0964 - IBD and Major Depression: Associated with Age, Sex, Smoking, Severity, and Extra-Intestinal Manifestations, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

