Sunday Poster Session
Category: IBD
P0966 - Early Real-World Patient Characteristics and Treatment Patterns in Upadacitinib-Treated Patients With Ulcerative Colitis: A U.S. Claims Database Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Corey A. Siegel, MD, MS
Dartmouth-Hitchcock Medical Center
Lebanon, NH
Presenting Author(s)
Ryan C. Ungaro, MD1, Jae Rok Kim, PharmD, MS2, Nidhi Shukla, PhD, MBA3, Parakkal Deepak, MBBS, MS4, Lisa Malter, MD5, Raymond K. Cross, MD, MS, FACG6, Cecile Holweg, PhD3, Valencia Remple, PhD7, Dolly Sharma, PhD3, Corey A.. Siegel, MD, MS8
1Icahn School of Medicine at Mount Sinai, New York, NY; 2AbbVie, Irvine, CA; 3AbbVie, Mettawa, IL; 4Washington University in St. Louis, St. Louis, MO; 5New York University Langone Health, New York, NY; 6Melissa L. Posner Institute for Digestive Health & Liver Disease at Mercy Medical Center, Baltimore, MD; 7AbbVie Inc., North Chicago, IL; 8Dartmouth-Hitchcock Medical Center, Lebanon, NH
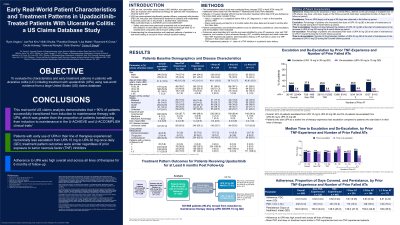
Introduction: Upadacitinib (UPA) has demonstrated efficacy in clinical trials and was approved in 2022 for treating adults with moderately to severely active ulcerative colitis (UC) in the US. Understanding real-world patient characteristics and treatment patterns is important to support clinical decision-making. This study describes the characteristics and early treatment patterns in patients with UC initiating UPA.
Methods: This retrospective cohort study was conducted from March 2022 to January 2024 using US healthcare claims data from the Merative™ MarketScan® Early View database. Patients ≥18 years initiating UPA 45 mg induction treatment (first date of fill was defined as index date) were included if they had ≥1 inpatient or 2 outpatient claims with a UC diagnosis (≥1 claim in the baseline period) and were continuously enrolled for ≥6 months before index date and 6 months after the index date. Patient characteristics and treatment patterns such as adherence (proportion of days covered [PDC], defined by percentage of available UPA days’ supply in the follow-up period), persistence, dose escalation, and de-escalation were evaluated. Outcomes were described at 6 months and were stratified by tumor necrosis factor inhibitor (TNFi) exposure and by prior line of advanced therapy (AT) including biologics and small molecules.
Results: A total of 452 patients were identified with 6 months of follow-up data. Mean age was 41 years, 46.5% were female, 74.8% were TNFi-experienced, and 58.8% had prior exposure to ≥2 ATs. Of 452 patients, 91.8% of patients moved from UPA 45mg induction to maintenance. Of these patients 27.7% received UPA 15 mg and 72.3% received UPA 30 mg. At 6 months, mean (standard deviation [SD]) PDC was 0.8 (0.2) and days on treatment was 150.5 (43.3) at 6 months (Table). In TNFi-experienced versus non-TNFi-experienced patients, mean PDC and days on treatment were similar. Overall, 27.0% of patients escalated dose from 15 to 30 mg and 3.7% de-escalated from 30 to 15 mg. Patients with 1 or 2 prior ATs had numerically better outcomes than those with 3 or 4 prior ATs.
Discussion: This real-world US claims analysis showed that a large proportion of patients remained on UPA from induction to maintenance. The 6-month adherence rate was comparable to estimates of other UC advanced therapies. Findings were consistent with the clinical response for UPA observed in clinical trials. Future analyses will evaluate outcomes with a longer follow-up period.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ryan C. Ungaro, MD1, Jae Rok Kim, PharmD, MS2, Nidhi Shukla, PhD, MBA3, Parakkal Deepak, MBBS, MS4, Lisa Malter, MD5, Raymond K. Cross, MD, MS, FACG6, Cecile Holweg, PhD3, Valencia Remple, PhD7, Dolly Sharma, PhD3, Corey A.. Siegel, MD, MS8. P0966 - Early Real-World Patient Characteristics and Treatment Patterns in Upadacitinib-Treated Patients With Ulcerative Colitis: A U.S. Claims Database Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai, New York, NY; 2AbbVie, Irvine, CA; 3AbbVie, Mettawa, IL; 4Washington University in St. Louis, St. Louis, MO; 5New York University Langone Health, New York, NY; 6Melissa L. Posner Institute for Digestive Health & Liver Disease at Mercy Medical Center, Baltimore, MD; 7AbbVie Inc., North Chicago, IL; 8Dartmouth-Hitchcock Medical Center, Lebanon, NH
Introduction: Upadacitinib (UPA) has demonstrated efficacy in clinical trials and was approved in 2022 for treating adults with moderately to severely active ulcerative colitis (UC) in the US. Understanding real-world patient characteristics and treatment patterns is important to support clinical decision-making. This study describes the characteristics and early treatment patterns in patients with UC initiating UPA.
Methods: This retrospective cohort study was conducted from March 2022 to January 2024 using US healthcare claims data from the Merative™ MarketScan® Early View database. Patients ≥18 years initiating UPA 45 mg induction treatment (first date of fill was defined as index date) were included if they had ≥1 inpatient or 2 outpatient claims with a UC diagnosis (≥1 claim in the baseline period) and were continuously enrolled for ≥6 months before index date and 6 months after the index date. Patient characteristics and treatment patterns such as adherence (proportion of days covered [PDC], defined by percentage of available UPA days’ supply in the follow-up period), persistence, dose escalation, and de-escalation were evaluated. Outcomes were described at 6 months and were stratified by tumor necrosis factor inhibitor (TNFi) exposure and by prior line of advanced therapy (AT) including biologics and small molecules.
Results: A total of 452 patients were identified with 6 months of follow-up data. Mean age was 41 years, 46.5% were female, 74.8% were TNFi-experienced, and 58.8% had prior exposure to ≥2 ATs. Of 452 patients, 91.8% of patients moved from UPA 45mg induction to maintenance. Of these patients 27.7% received UPA 15 mg and 72.3% received UPA 30 mg. At 6 months, mean (standard deviation [SD]) PDC was 0.8 (0.2) and days on treatment was 150.5 (43.3) at 6 months (Table). In TNFi-experienced versus non-TNFi-experienced patients, mean PDC and days on treatment were similar. Overall, 27.0% of patients escalated dose from 15 to 30 mg and 3.7% de-escalated from 30 to 15 mg. Patients with 1 or 2 prior ATs had numerically better outcomes than those with 3 or 4 prior ATs.
Discussion: This real-world US claims analysis showed that a large proportion of patients remained on UPA from induction to maintenance. The 6-month adherence rate was comparable to estimates of other UC advanced therapies. Findings were consistent with the clinical response for UPA observed in clinical trials. Future analyses will evaluate outcomes with a longer follow-up period.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ryan C. Ungaro: AbbVie – Advisory Committee/Board Member, Grant/Research Support. Boehringer Ingelheim – Grant/Research Support. Bristol Myers Squibb – Advisory Committee/Board Member. Celltrion – Advisory Committee/Board Member, Consultant. Eli Lilly – Grant/Research Support. Inotrem – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member, Grant/Research Support. Prometheus Labratories – Grant/Research Support. Roivant – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member.
Jae Rok Kim: AbbVie – Employee, Stock-publicly held company(excluding mutual/index funds).
Nidhi Shukla: AbbVie – Independent Contractor, Stock-publicly held company(excluding mutual/index funds).
Parakkal Deepak: AbbVie – Consultant, Grant/Research Support. Alimentiv – Grant/Research Support. Arena Pharmaceuticals – Grant/Research Support. Boehringer Ingelheim – Grant/Research Support. Bristol Myers Squibb-Celgene – Advisory Committee/Board Member, Grant/Research Support. CorEvitas LLC – Consultant. Janssen – Grant/Research Support. Pfizer – Grant/Research Support. Prometheus Biosciences – Grant/Research Support. Roche/Genentech – Advisory Committee/Board Member. Scipher Medicine – Grant/Research Support. Takeda – Grant/Research Support.
Lisa Malter: AbbVie – Advisory Committee/Board Member, Consultant, Grant/Research Support. Bristol Myers Squibb – Advisory Committee/Board Member. Celltrion – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member, Grant/Research Support. Merck – Advisory Committee/Board Member. Pfizer – Grant/Research Support. Takeda – Advisory Committee/Board Member, Grant/Research Support.
Raymond Cross: AbbVie – Consultant. Adiso – Consultant. Bristol Myers Squibb – Consultant. CorEvitas Registry – Scientific co-director. Fresenius Kabi – Consultant. Fzata – Consultant. IBD Education Group – Executive committee member. Janssen – Consultant, Grant/Research Support. Magellan Health – Consultant. Option Care Health – Consultant. Pfizer – Consultant. Pharmacosmos – Consultant. Samsung Bioepis – Consultant. Sandoz – Consultant. Sebela – Consultant. Takeda – Consultant.
Cecile Holweg: AbbVie – Employee, Stock-publicly held company(excluding mutual/index funds).
Valencia Remple: AbbVie – Employee, Stock-publicly held company(excluding mutual/index funds).
Dolly Sharma: AbbVie – Employee, Stock-publicly held company(excluding mutual/index funds).
Corey Siegel: Abbvie – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speaker for CME activities. BMS – Advisory Committee/Board Member, Consultant. Boomerang – Advisory Committee/Board Member, Consultant. Buhlman – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speaker for CME activities. Lilly – Advisory Committee/Board Member, Consultant. Napo pharmaceuticals – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Grant/Research Support, speaker for CME activities. Prometheus Biosciences – Advisory Committee/Board Member, Consultant. Prometheus Labs – Advisory Committee/Board Member, Consultant. Roivant – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support, speaker for CME activities. Trellus Health – Advisory Committee/Board Member, Consultant.
Ryan C. Ungaro, MD1, Jae Rok Kim, PharmD, MS2, Nidhi Shukla, PhD, MBA3, Parakkal Deepak, MBBS, MS4, Lisa Malter, MD5, Raymond K. Cross, MD, MS, FACG6, Cecile Holweg, PhD3, Valencia Remple, PhD7, Dolly Sharma, PhD3, Corey A.. Siegel, MD, MS8. P0966 - Early Real-World Patient Characteristics and Treatment Patterns in Upadacitinib-Treated Patients With Ulcerative Colitis: A U.S. Claims Database Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
