Sunday Poster Session
Category: IBD
P0973 - A Rare Complication: Tofacitinib-Induced Autoimmune Hemolytic Anemia in Ulcerative Colitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Rukaiya Bashir hamidu, MD
University of Maryland Medical Center
Baltimore, MD
Presenting Author(s)
Rukaiya Bashir hamidu, MD1, Lauren George, MD2
1University of Maryland Medical Center, Baltimore, MD; 2University of Maryland School of Medicine, Baltimore, MD
Introduction: Anemia is a common systemic manifestation of inflammatory bowel disease (IBD), typically due to nutritional deficiencies and chronic inflammation. Autoimmune hemolytic anemia (AIHA), a rare cause of anemia in IBD, occurs more frequently in ulcerative colitis (UC) than Crohn’s disease. Although AIHA has been linked to active UC and specific drug therapies, no cases have been associated with tofacitinib until now. We present a case of tofacitinib-induced AIHA in a UC patient, successfully treated with rituximab.
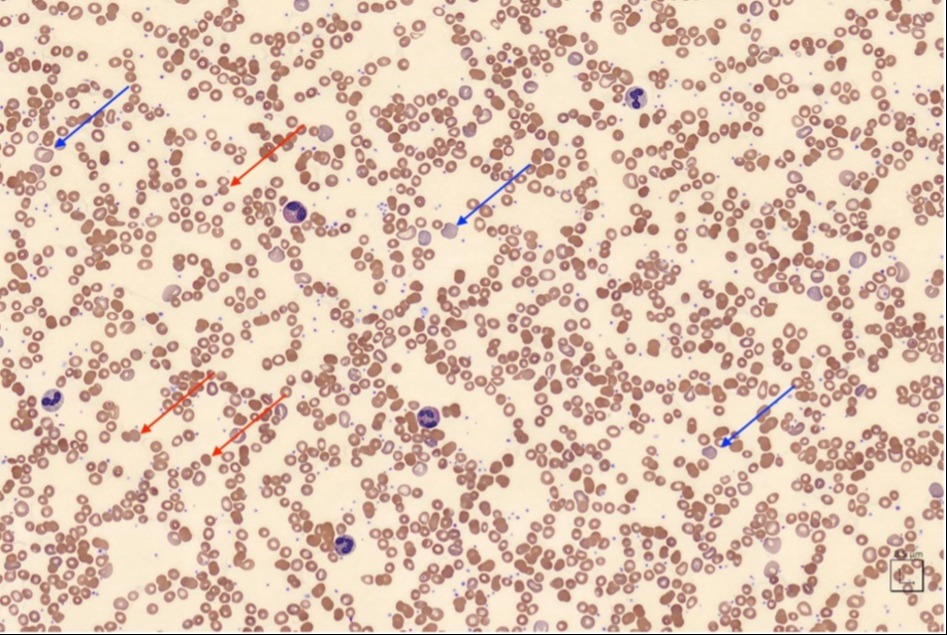
Case Description/Methods: A 45-year-old female with ulcerative pancolitis, diagnosed 17 months prior, presented to the IBD clinic with severe UC symptoms, including diarrhea, abdominal pain, and iron deficiency anemia (IDA), despite prior therapies with mesalamine, adalimumab, and vedolizumab. Initiating tofacitinib resolved her UC symptoms and IDA, but after 6 weeks, she developed severe anemia and recurrent IDA despite controlled colitis symptoms. Diagnostic tests for anemia, including a bone marrow biopsy and direct antiglobulin (Coombs) test, were normal. Suspecting bone marrow suppression from tofacitinib, it was discontinued, and ustekinumab was started for UC. Anemia persisted despite iron repletion, requiring frequent blood transfusions, prompting a referral to hematology. Peripheral blood smear revealed subtle signs of hemolysis, and subsequent testing confirmed warm AIHA (positive IgG Coombs test with panagglutinins on eluate test). Prednisone followed by rituximab resolved her anemia.
Discussion: AIHA involves antibody-triggered RBC destruction, primarily in the spleen (extravascular hemolysis), and is categorized as warm or cold, and primary or secondary. Diagnosis of AIHA is based on a positive Coombs test but coexistence with other anemia causes can complicate diagnosis. AIHA is often warm and secondary, commonly linked to active colitis or drug-induced by infliximab or sulfasalazine. Notably, there are no prior reported cases linking tofacitinib to AIHA. Treatment of AIHA in UC involves eliminating antibody production with glucocorticoids or immunomodulators like rituximab. In refractory cases, splenectomy or colectomy can resolve hemolysis. This case highlights AIHA as an insidious complication of UC, triggered by tofacitinib in this patient, and underscores the challenge of diagnosing AIHA amidst more common causes of anemia. Furthermore, considering AIHA in the differential diagnosis for anemia in UC is crucial for timely initiation of appropriate treatment.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rukaiya Bashir hamidu, MD1, Lauren George, MD2. P0973 - A Rare Complication: Tofacitinib-Induced Autoimmune Hemolytic Anemia in Ulcerative Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Maryland Medical Center, Baltimore, MD; 2University of Maryland School of Medicine, Baltimore, MD
Introduction: Anemia is a common systemic manifestation of inflammatory bowel disease (IBD), typically due to nutritional deficiencies and chronic inflammation. Autoimmune hemolytic anemia (AIHA), a rare cause of anemia in IBD, occurs more frequently in ulcerative colitis (UC) than Crohn’s disease. Although AIHA has been linked to active UC and specific drug therapies, no cases have been associated with tofacitinib until now. We present a case of tofacitinib-induced AIHA in a UC patient, successfully treated with rituximab.
Case Description/Methods: A 45-year-old female with ulcerative pancolitis, diagnosed 17 months prior, presented to the IBD clinic with severe UC symptoms, including diarrhea, abdominal pain, and iron deficiency anemia (IDA), despite prior therapies with mesalamine, adalimumab, and vedolizumab. Initiating tofacitinib resolved her UC symptoms and IDA, but after 6 weeks, she developed severe anemia and recurrent IDA despite controlled colitis symptoms. Diagnostic tests for anemia, including a bone marrow biopsy and direct antiglobulin (Coombs) test, were normal. Suspecting bone marrow suppression from tofacitinib, it was discontinued, and ustekinumab was started for UC. Anemia persisted despite iron repletion, requiring frequent blood transfusions, prompting a referral to hematology. Peripheral blood smear revealed subtle signs of hemolysis, and subsequent testing confirmed warm AIHA (positive IgG Coombs test with panagglutinins on eluate test). Prednisone followed by rituximab resolved her anemia.
Discussion: AIHA involves antibody-triggered RBC destruction, primarily in the spleen (extravascular hemolysis), and is categorized as warm or cold, and primary or secondary. Diagnosis of AIHA is based on a positive Coombs test but coexistence with other anemia causes can complicate diagnosis. AIHA is often warm and secondary, commonly linked to active colitis or drug-induced by infliximab or sulfasalazine. Notably, there are no prior reported cases linking tofacitinib to AIHA. Treatment of AIHA in UC involves eliminating antibody production with glucocorticoids or immunomodulators like rituximab. In refractory cases, splenectomy or colectomy can resolve hemolysis. This case highlights AIHA as an insidious complication of UC, triggered by tofacitinib in this patient, and underscores the challenge of diagnosing AIHA amidst more common causes of anemia. Furthermore, considering AIHA in the differential diagnosis for anemia in UC is crucial for timely initiation of appropriate treatment.
Figure: Figure 1. Peripheral blood smear (PBS) from the patient showing spherocytes (marked by red arrows), a common feature in warm autoimmune hemolytic anemia (AIHA). The smear also exhibits anisocytosis and increased reticulocytes (appearing as macrocytic cells with a bluish hue, marked by blue arrows), indicating an erythropoietic response to hematinics (iron and folate). These findings, alongside normal iron, B12, and folate levels, raised suspicion for hemolysis, prompting hemolytic anemia testing which resulted positive for warm AIHA. Of note, schistocytes are not typically observed in the PBS in cases of warm AIHA as the hemolysis primarily takes place in the spleen (i.e., extravascular hemolysis).
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rukaiya Bashir hamidu indicated no relevant financial relationships.
Lauren George: Janssen – Advisory Committee/Board Member.
Rukaiya Bashir hamidu, MD1, Lauren George, MD2. P0973 - A Rare Complication: Tofacitinib-Induced Autoimmune Hemolytic Anemia in Ulcerative Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
