Sunday Poster Session
Category: IBD
P0974 - Unmasking Opioid Use Disorder: Navigating Diagnostic Challenges and Stigma in Gastrointestinal Cases
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- MY
Marcel J. Yibirin, MD, MPH
Boston Medical Center, Boston University School of Medicine
Boston, MA
Presenting Author(s)
Matthew Ryan, BS1, Marcel J. Yibirin, MD, MPH2, Sebastian Suarez, MD, MPH3
1University of Miami Miller School of Medicine, Miami, FL; 2Boston Medical Center, Boston University School of Medicine, Boston, MA; 3University of Miami Health System, Miami, FL
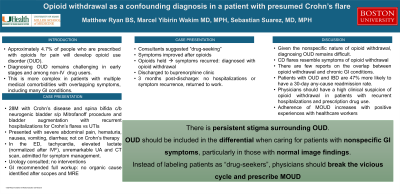
Introduction: Opioid use disorder (OUD) affects over 2 million people in the United States, with a significant proportion originating from physicians’ prescriptions. Diagnosing OUD particularly challenging, especially in the early stages and among non-intravenous drug users. The complexity is further amplified in patients with multiple medical comorbidities, as overlapping symptoms can obscure the distinction between opioid withdrawal and other potential causes, necessitating careful diagnostic consideration.
Case Description/Methods: A 28-year-old male with Crohn’s disease and spina bifida complicated by neurogenic bladder and status post Mirtanoff procedure and bladder augmentation, with monthly hospitalizations for Crohn’s flares and urinary tract infections (UTI) was admitted with severe abdominal pain, hematuria, nausea, vomiting, and diarrhea. Workup including CBC, CMP, UA, blood and urine cultures, CT scan of the abdomen and pelvis, upper endoscopy, colonoscopy, and MRI enterography did not identify an organic cause of the symptoms. The GI consultant service ruled out a Crohn’s flare and dismissed the case as “drug-seeking behavior”. The patient's symptoms improved within 48 hours of admission, coinciding with opioid administration for pain management, after which the patient was diagnosed with opioid withdrawal. Opioids were subsequently discontinued, leading to recurrence of symptoms within 24 hours. Following this diagnosis, the patient was discharged with a scheduled appointment to start buprenorphine as treatment for OUD. Three months post-discharge, the patient remained free from hospitalizations and symptom recurrence, and regained all functionality.
Discussion: This case highlights the persistent stigma surrounding OUD within medical communities, despite increased public awareness. Instead of labeling patients as “drug-seekers”, physicians should adopt a holistic approach and consider OUD as a treatable medical condition. Given the overlap of GI symptoms between opioid withdrawal and conditions like Crohn’s disease, it is especially important for gastroenterologists and hospitalists to include OUD as a differential diagnoses, particularly in patients with normal image findings. This approach can lead to earlier recognition of OUD, expedited diagnosis, resource conservation, and potentially reduction in mortality attributed to overdose. Finally, this case underscores the clinical and psychosocial benefits of medications for OUD.
Disclosures:
Matthew Ryan, BS1, Marcel J. Yibirin, MD, MPH2, Sebastian Suarez, MD, MPH3. P0974 - Unmasking Opioid Use Disorder: Navigating Diagnostic Challenges and Stigma in Gastrointestinal Cases, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Miami Miller School of Medicine, Miami, FL; 2Boston Medical Center, Boston University School of Medicine, Boston, MA; 3University of Miami Health System, Miami, FL
Introduction: Opioid use disorder (OUD) affects over 2 million people in the United States, with a significant proportion originating from physicians’ prescriptions. Diagnosing OUD particularly challenging, especially in the early stages and among non-intravenous drug users. The complexity is further amplified in patients with multiple medical comorbidities, as overlapping symptoms can obscure the distinction between opioid withdrawal and other potential causes, necessitating careful diagnostic consideration.
Case Description/Methods: A 28-year-old male with Crohn’s disease and spina bifida complicated by neurogenic bladder and status post Mirtanoff procedure and bladder augmentation, with monthly hospitalizations for Crohn’s flares and urinary tract infections (UTI) was admitted with severe abdominal pain, hematuria, nausea, vomiting, and diarrhea. Workup including CBC, CMP, UA, blood and urine cultures, CT scan of the abdomen and pelvis, upper endoscopy, colonoscopy, and MRI enterography did not identify an organic cause of the symptoms. The GI consultant service ruled out a Crohn’s flare and dismissed the case as “drug-seeking behavior”. The patient's symptoms improved within 48 hours of admission, coinciding with opioid administration for pain management, after which the patient was diagnosed with opioid withdrawal. Opioids were subsequently discontinued, leading to recurrence of symptoms within 24 hours. Following this diagnosis, the patient was discharged with a scheduled appointment to start buprenorphine as treatment for OUD. Three months post-discharge, the patient remained free from hospitalizations and symptom recurrence, and regained all functionality.
Discussion: This case highlights the persistent stigma surrounding OUD within medical communities, despite increased public awareness. Instead of labeling patients as “drug-seekers”, physicians should adopt a holistic approach and consider OUD as a treatable medical condition. Given the overlap of GI symptoms between opioid withdrawal and conditions like Crohn’s disease, it is especially important for gastroenterologists and hospitalists to include OUD as a differential diagnoses, particularly in patients with normal image findings. This approach can lead to earlier recognition of OUD, expedited diagnosis, resource conservation, and potentially reduction in mortality attributed to overdose. Finally, this case underscores the clinical and psychosocial benefits of medications for OUD.
Disclosures:
Matthew Ryan indicated no relevant financial relationships.
Marcel Yibirin indicated no relevant financial relationships.
Sebastian Suarez indicated no relevant financial relationships.
Matthew Ryan, BS1, Marcel J. Yibirin, MD, MPH2, Sebastian Suarez, MD, MPH3. P0974 - Unmasking Opioid Use Disorder: Navigating Diagnostic Challenges and Stigma in Gastrointestinal Cases, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
