Sunday Poster Session
Category: IBD
P0979 - Autoimmune Hemolytic Anemia as an Extraintestinal Manifestation of Inflammatory Bowel Disease
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- AC
Aastha Chokshi, MD
The Warren Alpert Medical School of Brown University
Plainsboro, NJ
Presenting Author(s)
Aastha Chokshi, MD1, Sean Fine, MD2
1The Warren Alpert Medical School of Brown University, Plainsboro, NJ; 2Brown Medicine/Lifespan, Providence, RI
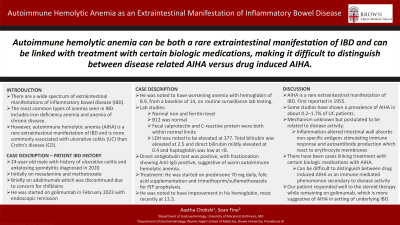
Introduction: There are a wide spectrum of extraintestinal manifestations of inflammatory bowel disease (IBD). Anemia is commonly associated with IBD. The most common types of anemia seen in IBD includes iron deficiency anemia and anemia of chronic disease. However, autoimmune hemolytic anemia (AIHA) is a rare extraintestinal manifestation of IBD and is more commonly associated with ulcerative colitis (UC) than Crohn’s disease (CD). We describe a case of warm autoimmune hemolytic anemia (WAHA) associated with ulcerative colitis.
Case Description/Methods: Patient is a 24-year-old male with history of ulcerative colitis, initially diagnosed in 2020, as well as ankylosing spondylitis currently on golimumab 100 mg/ml every 4 weeks presented with worsening anemia. He was initially diagnosed with ulcerative colitis in 2020 with autoimmune arthritis and was initially on mesalamine and methotrexate. He was briefly on adalimumab which was discontinued due to concern for chilblains. He was started on golimumab in February 2023 with endoscopic remission. He was noted to have worsening anemia with hemoglobin of 8.9 in Spring 2024, from a baseline of 14. Iron studies showed a normal iron and ferritin level, B12 was normal. Fecal calprotectin and C-reactive protein were both within normal limits. LDH was noted to be elevated at 377. Total bilirubin was elevated at 2.5 and direct bilirubin mildly elevated at 0.4 and haptoglobin was low at < 8. Direct antiglobulin test was positive, with fractionation showing Anti-IgG positive, suggestive of warm autoimmune hemolytic anemia. He was started on prednisone 70 mg daily, folic acid supplementation and trimethoprim/sulfamethoxazole for PJP prophylaxis. He was noted to have improvement in his hemoglobin, most recently at 13.3.
Discussion: Our case highlights an instance of a rare extraintestinal manifestation of IBD. Some studies have shown a prevalence of AIHA in about 0.2–1.7% of UC patients. AIHA in IBD patients was first reported in 1955 when four cases of female patients with UC and AIHA were reported. At the same time, there have been cases linking treatment with certain biologic medications with AIHA and this can be difficult to distinguish between drug induced AIHA vs and immune mediated phenomenon secondary to disease activity. Our patient responded well to the steroid therapy while remaining on golimumab, which is more suggestive of AIHA in setting of underlying IBD as opposed to drug induced phenomenon.
Disclosures:
Aastha Chokshi, MD1, Sean Fine, MD2. P0979 - Autoimmune Hemolytic Anemia as an Extraintestinal Manifestation of Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The Warren Alpert Medical School of Brown University, Plainsboro, NJ; 2Brown Medicine/Lifespan, Providence, RI
Introduction: There are a wide spectrum of extraintestinal manifestations of inflammatory bowel disease (IBD). Anemia is commonly associated with IBD. The most common types of anemia seen in IBD includes iron deficiency anemia and anemia of chronic disease. However, autoimmune hemolytic anemia (AIHA) is a rare extraintestinal manifestation of IBD and is more commonly associated with ulcerative colitis (UC) than Crohn’s disease (CD). We describe a case of warm autoimmune hemolytic anemia (WAHA) associated with ulcerative colitis.
Case Description/Methods: Patient is a 24-year-old male with history of ulcerative colitis, initially diagnosed in 2020, as well as ankylosing spondylitis currently on golimumab 100 mg/ml every 4 weeks presented with worsening anemia. He was initially diagnosed with ulcerative colitis in 2020 with autoimmune arthritis and was initially on mesalamine and methotrexate. He was briefly on adalimumab which was discontinued due to concern for chilblains. He was started on golimumab in February 2023 with endoscopic remission. He was noted to have worsening anemia with hemoglobin of 8.9 in Spring 2024, from a baseline of 14. Iron studies showed a normal iron and ferritin level, B12 was normal. Fecal calprotectin and C-reactive protein were both within normal limits. LDH was noted to be elevated at 377. Total bilirubin was elevated at 2.5 and direct bilirubin mildly elevated at 0.4 and haptoglobin was low at < 8. Direct antiglobulin test was positive, with fractionation showing Anti-IgG positive, suggestive of warm autoimmune hemolytic anemia. He was started on prednisone 70 mg daily, folic acid supplementation and trimethoprim/sulfamethoxazole for PJP prophylaxis. He was noted to have improvement in his hemoglobin, most recently at 13.3.
Discussion: Our case highlights an instance of a rare extraintestinal manifestation of IBD. Some studies have shown a prevalence of AIHA in about 0.2–1.7% of UC patients. AIHA in IBD patients was first reported in 1955 when four cases of female patients with UC and AIHA were reported. At the same time, there have been cases linking treatment with certain biologic medications with AIHA and this can be difficult to distinguish between drug induced AIHA vs and immune mediated phenomenon secondary to disease activity. Our patient responded well to the steroid therapy while remaining on golimumab, which is more suggestive of AIHA in setting of underlying IBD as opposed to drug induced phenomenon.
Disclosures:
Aastha Chokshi indicated no relevant financial relationships.
Sean Fine: Abbvie – Advisory Committee/Board Member. Bristol Myers Squibb – Consultant. Takeda – Advisory Committee/Board Member.
Aastha Chokshi, MD1, Sean Fine, MD2. P0979 - Autoimmune Hemolytic Anemia as an Extraintestinal Manifestation of Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
