Sunday Poster Session
Category: IBD
P0984 - Challenges of Pyoderma Gangrenosum Diagnosis in the Dark Skin Population
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Iyad Al-Bustami, MD, MPH(c)
Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Iyad Al-bustami, MD, MPH(c)1, Shamsa M. Qaadri, BSc2, Shafiq Qaadri, BA3, Amogh R. Kare, BS2, Deepak Kumar Palanichami, BSc4, Saira Shah, MD5, Saigopal R. Gujjula, MD5, Kenan Alrejjal, MBBS6, Rasha H. Saleh, MD5, Anuj R. Sharma, MBBS5, Francis Gacek, DO5, Sweta Lohani, MBBS, MD5, Manasa Ginjupalli, MBBS, MD7, Naresh Kumar, MD8, Vikash Kumar, MD9, Camelia Ciobanu, MD5, Amr Dokmak, MD5, Ali Wakil, MD5, Denzil Etienne, MD5, Madhavi Reddy, MD, FACG5
1Brooklyn Hospital Center, Houston, TX; 2St. George's University School of Medicine, Brooklyn, NY; 3Toronto Metropolitan University, Toronto, ON, Canada; 4St. George's University School of Medicine, Hannon, ON, Canada; 5Brooklyn Hospital Center, Brooklyn, NY; 6MedStar Health-Georgetown/Washington Hospital Center, Washington, DC; 7The Brooklyn Hospital Center, New York, NY; 8The Brooklyn Hospital Center, Brooklyn, NY; 9Creighton University School of Medicine, Brooklyn, NY
Introduction: Pyoderma gangrenosum (PG) is an autoinflammatory skin disease characterized by ulcerative lesions in soft tissue and the skin. While its etiology remains unknown, it is associated with systemic inflammatory diseases in up to 50% of cases. The estimated incidence of PG in the United States ranges from 6-20 cases per 100,000 individuals. Due to the absence of a definitive test, PG is frequently misdiagnosed or considered erroneously to have infectious or gangrenous origin. The following case report demonstrates the necessity of considering clinical presentations potentially overlooked due to racial bias and ethno-dermatological factors.
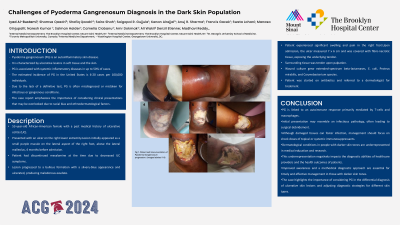
Case Description/Methods: A 53-year-old African-American female with a past medical history of ulcerative colitis (UC) who presented with an ulcer on the right lower extremity. The lesion initially appeared as a small purple macule on the lateral aspect of the right foot superior to the lateral malleolus 4 months prior to admission. The patient had discontinued mesalamine at this time due to decreased symptoms of UC. The lesion progressed to bullous formation with a silvery-blue appearance and subsequently ulcerated, producing malodorous exudate. The patient experienced significant swelling and pain in the right foot. Upon admission, the ulcer measured 7 x 6 cm and was covered with fibro-necrotic tissue exposing the underlying tendon. Surrounding tissue was tender upon palpation. A wound culture grew extended-spectrum beta-lactamases, E. coli, Proteus mirabilis, and Corynebacterium species. The patient was started on antibiotics and referred to a dermatologist for treatment.
Discussion: PG is linked to an autoimmune response mediated by T-cells mainly and macrophages. Initial presentation of PG can be attributed to an infectious pathology leading the patient to undergo surgical debridement. While damaged tissues can foster an infection, the mainstay of management should be a shock dose of topical or systemic immunosuppressants. Dermatological conditions in people with darker skin tones are underrepresented in medical education and research, which negatively influences the diagnostic ability of healthcare providers and health outcomes of patients. Improved awareness in those with darker skin tones and a methodical approach to diagnosis are crucial for timely and effective management. This case underscores the importance of considering PG in the differential diagnosis of ulcerative skin lesions and adapting diagnostic strategies to account for skin type.

Disclosures:
Iyad Al-bustami, MD, MPH(c)1, Shamsa M. Qaadri, BSc2, Shafiq Qaadri, BA3, Amogh R. Kare, BS2, Deepak Kumar Palanichami, BSc4, Saira Shah, MD5, Saigopal R. Gujjula, MD5, Kenan Alrejjal, MBBS6, Rasha H. Saleh, MD5, Anuj R. Sharma, MBBS5, Francis Gacek, DO5, Sweta Lohani, MBBS, MD5, Manasa Ginjupalli, MBBS, MD7, Naresh Kumar, MD8, Vikash Kumar, MD9, Camelia Ciobanu, MD5, Amr Dokmak, MD5, Ali Wakil, MD5, Denzil Etienne, MD5, Madhavi Reddy, MD, FACG5. P0984 - Challenges of Pyoderma Gangrenosum Diagnosis in the Dark Skin Population, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Brooklyn Hospital Center, Houston, TX; 2St. George's University School of Medicine, Brooklyn, NY; 3Toronto Metropolitan University, Toronto, ON, Canada; 4St. George's University School of Medicine, Hannon, ON, Canada; 5Brooklyn Hospital Center, Brooklyn, NY; 6MedStar Health-Georgetown/Washington Hospital Center, Washington, DC; 7The Brooklyn Hospital Center, New York, NY; 8The Brooklyn Hospital Center, Brooklyn, NY; 9Creighton University School of Medicine, Brooklyn, NY
Introduction: Pyoderma gangrenosum (PG) is an autoinflammatory skin disease characterized by ulcerative lesions in soft tissue and the skin. While its etiology remains unknown, it is associated with systemic inflammatory diseases in up to 50% of cases. The estimated incidence of PG in the United States ranges from 6-20 cases per 100,000 individuals. Due to the absence of a definitive test, PG is frequently misdiagnosed or considered erroneously to have infectious or gangrenous origin. The following case report demonstrates the necessity of considering clinical presentations potentially overlooked due to racial bias and ethno-dermatological factors.
Case Description/Methods: A 53-year-old African-American female with a past medical history of ulcerative colitis (UC) who presented with an ulcer on the right lower extremity. The lesion initially appeared as a small purple macule on the lateral aspect of the right foot superior to the lateral malleolus 4 months prior to admission. The patient had discontinued mesalamine at this time due to decreased symptoms of UC. The lesion progressed to bullous formation with a silvery-blue appearance and subsequently ulcerated, producing malodorous exudate. The patient experienced significant swelling and pain in the right foot. Upon admission, the ulcer measured 7 x 6 cm and was covered with fibro-necrotic tissue exposing the underlying tendon. Surrounding tissue was tender upon palpation. A wound culture grew extended-spectrum beta-lactamases, E. coli, Proteus mirabilis, and Corynebacterium species. The patient was started on antibiotics and referred to a dermatologist for treatment.
Discussion: PG is linked to an autoimmune response mediated by T-cells mainly and macrophages. Initial presentation of PG can be attributed to an infectious pathology leading the patient to undergo surgical debridement. While damaged tissues can foster an infection, the mainstay of management should be a shock dose of topical or systemic immunosuppressants. Dermatological conditions in people with darker skin tones are underrepresented in medical education and research, which negatively influences the diagnostic ability of healthcare providers and health outcomes of patients. Improved awareness in those with darker skin tones and a methodical approach to diagnosis are crucial for timely and effective management. This case underscores the importance of considering PG in the differential diagnosis of ulcerative skin lesions and adapting diagnostic strategies to account for skin type.

Figure: Fig.1 Patient Self-documentation of Pyoderma Gangrenosum Progression. (images labeled 1-9)
Disclosures:
Iyad Al-bustami indicated no relevant financial relationships.
Shamsa Qaadri indicated no relevant financial relationships.
Shafiq Qaadri indicated no relevant financial relationships.
Amogh Kare indicated no relevant financial relationships.
Deepak Kumar Palanichami indicated no relevant financial relationships.
Saira Shah indicated no relevant financial relationships.
Saigopal Gujjula indicated no relevant financial relationships.
Kenan Alrejjal indicated no relevant financial relationships.
Rasha Saleh indicated no relevant financial relationships.
Anuj Sharma indicated no relevant financial relationships.
Francis Gacek indicated no relevant financial relationships.
Sweta Lohani indicated no relevant financial relationships.
Manasa Ginjupalli indicated no relevant financial relationships.
Naresh Kumar indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Camelia Ciobanu indicated no relevant financial relationships.
Amr Dokmak indicated no relevant financial relationships.
Ali Wakil indicated no relevant financial relationships.
Denzil Etienne indicated no relevant financial relationships.
Madhavi Reddy indicated no relevant financial relationships.
Iyad Al-bustami, MD, MPH(c)1, Shamsa M. Qaadri, BSc2, Shafiq Qaadri, BA3, Amogh R. Kare, BS2, Deepak Kumar Palanichami, BSc4, Saira Shah, MD5, Saigopal R. Gujjula, MD5, Kenan Alrejjal, MBBS6, Rasha H. Saleh, MD5, Anuj R. Sharma, MBBS5, Francis Gacek, DO5, Sweta Lohani, MBBS, MD5, Manasa Ginjupalli, MBBS, MD7, Naresh Kumar, MD8, Vikash Kumar, MD9, Camelia Ciobanu, MD5, Amr Dokmak, MD5, Ali Wakil, MD5, Denzil Etienne, MD5, Madhavi Reddy, MD, FACG5. P0984 - Challenges of Pyoderma Gangrenosum Diagnosis in the Dark Skin Population, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
