Sunday Poster Session
Category: IBD
P1015 - Rare Case of Immune Checkpoint Inhibitor Colitis Manifesting as Pneumatosis Intestinalis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- AD
Apaar Dadlani, MBBS
Houston Methodist Hospital
Houston, TX
Presenting Author(s)
Apaar Dadlani, MBBS1, Mary R. Schwartz, MD1, Christopher Fan, MD2, Neha Mathur, MD1
1Houston Methodist Hospital, Houston, TX; 2Underwood Center for Digestive Disorders, Houston Methodist Hospital, Houston, TX
Introduction: Pneumatosis intestinalis (PI) is a rare complication of anti-cancer therapies. Pembrolizumab is an anti-PD1 monoclonal antibody, known to cause enterocolitis as an immune-related adverse event (iRAE). We present a rare case of pembrolizumab related colitis manifesting as pneumatosis intestinalis.
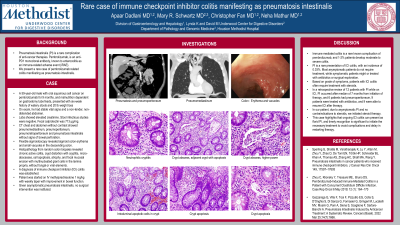
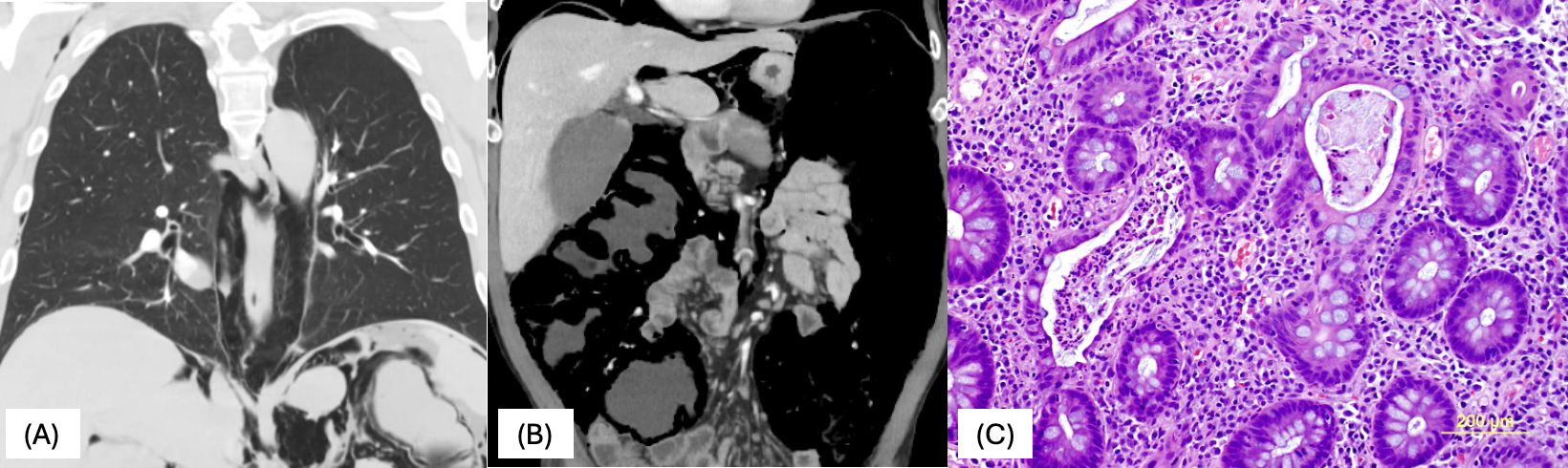
Case Description/Methods: A 59-year-old male with oral squamous cell carcinoma on pembrolizumab for 9 months, and malnutrition dependent on gastrostomy tube feeds, presented with six-week history of watery stools and 20 lb weight loss. On exam, he had stable vital signs and a non-tender, non-distended abdomen. Labs showed elevated creatinine. Stool infectious studies were negative. Fecal calprotectin was 713 μg/mg. CT chest and abdomen without contrast showed pneumomediastinum, pneumoperitoneum, pneumoretroperitoneum and pneumatosis intestinalis without signs of bowel perforation. Flexible sigmoidoscopy revealed sigmoid colon erythema and small vacuoles in the descending colon. Random colon biopsies demonstrated features of chronic active colitis with crypt distortion, neutrophilic cryptitis, crypt abscesses, crypt epithelial apoptosis, focal mucosal erosion, and focal multinucleated giant cells in the lamina propria. No fungus or viral cytopathic effect was seen. A diagnosis of immune checkpoint inhibitor (ICI) colitis was made, and the patient was started on IV methylprednisolone 1 mg/kg with weekly taper with improvement in bowel function. Given asymptomatic PI, no surgical intervention was instituted.
Discussion: ICI colitis is a rare known iRAE of pembrolizumab, and 1-2% of patients develop moderate to severe colitis. PI is a rare presentation of ICI colitis, with an incidence of 0.03%. Most asymptomatic patients do not require treatment, while symptomatic patients can be treated with antibiotics or surgical exploration. Based on the grade of symptoms, patients with ICI colitis often require treatment with steroids. In a retrospective review of 12 patients with PI while on ICI, PI occurred after a median of 7 months from initiation of therapy. 6 patients had pneumoperitoneum, 9 patients were treated with antibiotics, and 9 were able to resume ICI after therapy. In our patient, due to asymptomatic PI and no contraindications to steroids, we initiated steroid therapy to treat the underlying colitis. This case highlights that ongoing ICI colitis can present as florid PI, and timely recognition is significant to initiate the necessary treatment to avoid complications and delay in restarting therapy.
Disclosures:
Apaar Dadlani, MBBS1, Mary R. Schwartz, MD1, Christopher Fan, MD2, Neha Mathur, MD1. P1015 - Rare Case of Immune Checkpoint Inhibitor Colitis Manifesting as Pneumatosis Intestinalis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Houston Methodist Hospital, Houston, TX; 2Underwood Center for Digestive Disorders, Houston Methodist Hospital, Houston, TX
Introduction: Pneumatosis intestinalis (PI) is a rare complication of anti-cancer therapies. Pembrolizumab is an anti-PD1 monoclonal antibody, known to cause enterocolitis as an immune-related adverse event (iRAE). We present a rare case of pembrolizumab related colitis manifesting as pneumatosis intestinalis.
Case Description/Methods: A 59-year-old male with oral squamous cell carcinoma on pembrolizumab for 9 months, and malnutrition dependent on gastrostomy tube feeds, presented with six-week history of watery stools and 20 lb weight loss. On exam, he had stable vital signs and a non-tender, non-distended abdomen. Labs showed elevated creatinine. Stool infectious studies were negative. Fecal calprotectin was 713 μg/mg. CT chest and abdomen without contrast showed pneumomediastinum, pneumoperitoneum, pneumoretroperitoneum and pneumatosis intestinalis without signs of bowel perforation. Flexible sigmoidoscopy revealed sigmoid colon erythema and small vacuoles in the descending colon. Random colon biopsies demonstrated features of chronic active colitis with crypt distortion, neutrophilic cryptitis, crypt abscesses, crypt epithelial apoptosis, focal mucosal erosion, and focal multinucleated giant cells in the lamina propria. No fungus or viral cytopathic effect was seen. A diagnosis of immune checkpoint inhibitor (ICI) colitis was made, and the patient was started on IV methylprednisolone 1 mg/kg with weekly taper with improvement in bowel function. Given asymptomatic PI, no surgical intervention was instituted.
Discussion: ICI colitis is a rare known iRAE of pembrolizumab, and 1-2% of patients develop moderate to severe colitis. PI is a rare presentation of ICI colitis, with an incidence of 0.03%. Most asymptomatic patients do not require treatment, while symptomatic patients can be treated with antibiotics or surgical exploration. Based on the grade of symptoms, patients with ICI colitis often require treatment with steroids. In a retrospective review of 12 patients with PI while on ICI, PI occurred after a median of 7 months from initiation of therapy. 6 patients had pneumoperitoneum, 9 patients were treated with antibiotics, and 9 were able to resume ICI after therapy. In our patient, due to asymptomatic PI and no contraindications to steroids, we initiated steroid therapy to treat the underlying colitis. This case highlights that ongoing ICI colitis can present as florid PI, and timely recognition is significant to initiate the necessary treatment to avoid complications and delay in restarting therapy.
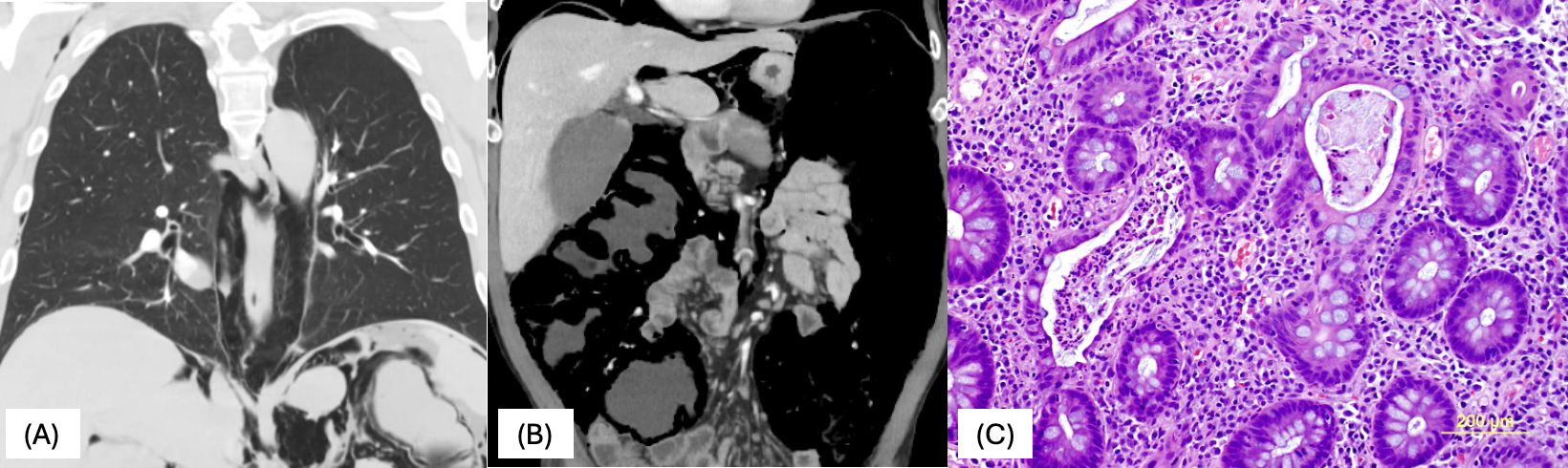
Figure: (A) CT chest demonstrating pneumomediastinum
(B) CT abdomen demonstrating pneumoperitoneum and pneumatosis intestinalis
(C) Photomicrograph of colon biopsy demonstrating a crypt abscess to the left and a dilated crypt with intraluminal apoptotic tumor cells to the right (H and E, original magnification x200), interpreted as compatible with immune checkpoint inhibitor colitis
(B) CT abdomen demonstrating pneumoperitoneum and pneumatosis intestinalis
(C) Photomicrograph of colon biopsy demonstrating a crypt abscess to the left and a dilated crypt with intraluminal apoptotic tumor cells to the right (H and E, original magnification x200), interpreted as compatible with immune checkpoint inhibitor colitis
Disclosures:
Apaar Dadlani indicated no relevant financial relationships.
Mary Schwartz indicated no relevant financial relationships.
Christopher Fan indicated no relevant financial relationships.
Neha Mathur: Ardelyx – Advisory Committee/Board Member. Sanofi and Regenernon – Advisory Committee/Board Member, Speakers Bureau.
Apaar Dadlani, MBBS1, Mary R. Schwartz, MD1, Christopher Fan, MD2, Neha Mathur, MD1. P1015 - Rare Case of Immune Checkpoint Inhibitor Colitis Manifesting as Pneumatosis Intestinalis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
