Sunday Poster Session
Category: IBD
P1020 - Extranodal Marginal Zone Lymphoma of Mucosa-Associated Lymphoid Tissue of the Stomach and Small Intestine Mimicking Crohn’s Disease With Suspected Transformation to Diffuse Large B-Cell Lymphoma
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- AH
Anam Herekar, MD
Augusta University
Augusta, GA
Presenting Author(s)
Anam Herekar, MD1, Menna Megahed, MD2, Harshitha Addagatla, MD3, Evangelos Tsipotis, MD3
1Augusta University, Augusta, GA; 2Augusta, GA; 3Augusta University Medical Center, Augusta, GA
Introduction: Extranodal marginal zone mucosa-associated lymphoma (MALT), is a form of non-Hodgkin’s lymphoma most commonly found in stomach. (1) Rarely, it can be seen in the small intestine and can progress to Diffuse large B-cell lymphoma (DLBCL). (1) It can mimic Crohn’s Disease (CD) delaying diagnosis. We present a rare case of marginal zone MALT lymphoma mimicking CD with suspected transformation to DLBCL.
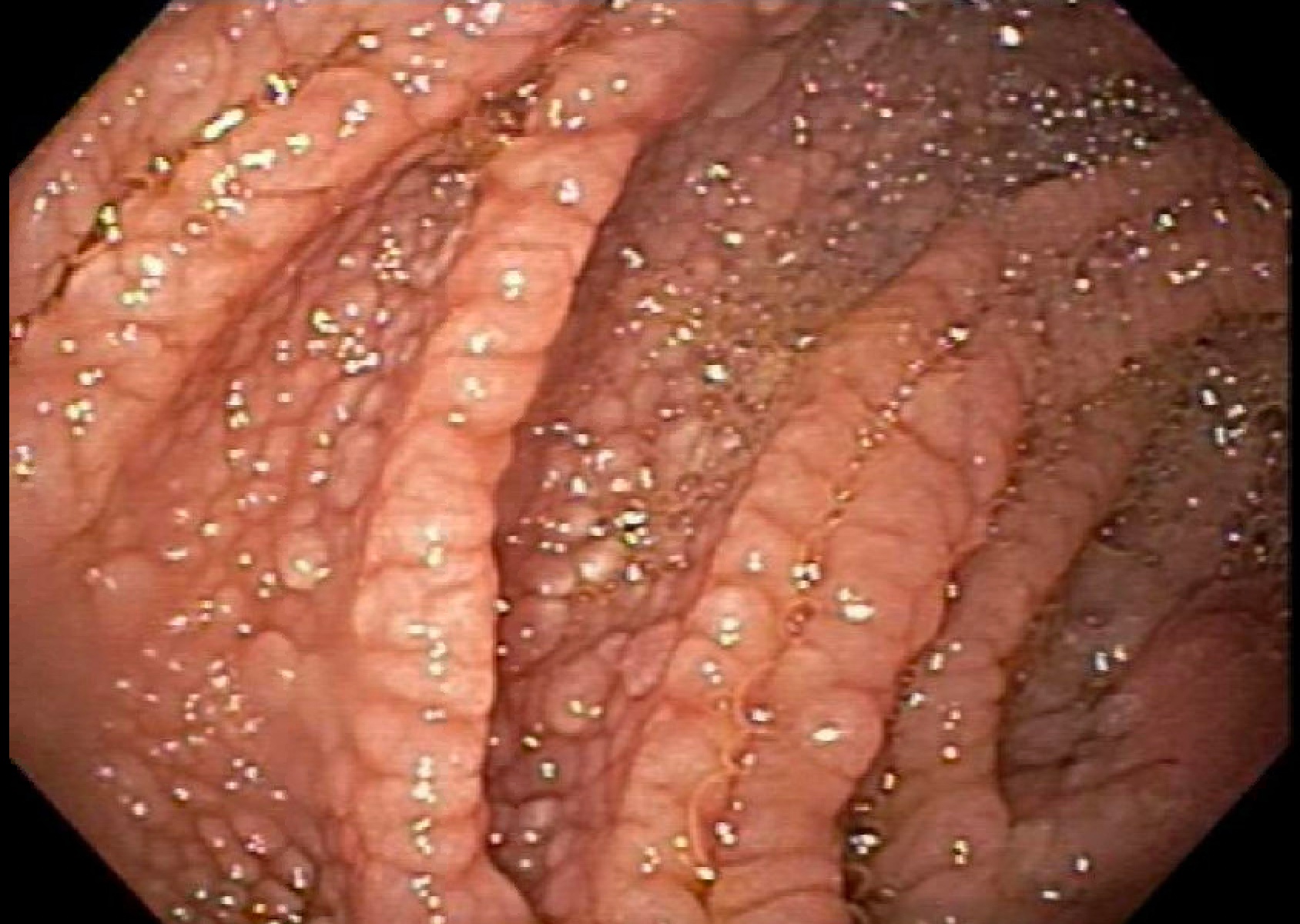
Case Description/Methods: 42-year-old male presented to gastroenterology clinic with weight loss, chronic lower extremity edema and diarrhea. Labs with albumin < 1.5 mg/dL elevated IgA with low IgG and IgM, Quantiferon negative, ESR 110 mm/hr and CRP 3.2 mg/dL, Calprotectin >800 ug/g, and low fecal elastase. Stool studies positive for EPEC/EAEC treated with azithromycin. Endoscopic evaluation showed nodular gastric and duodenal mucosa, a large duodenal bulb ulcer, nodular mucosa of the terminal ileum (TI) and rectal erythema. Pathology showed chronic gastritis, chronic active cryptitis in duodenum and TI, and chronic colitis in the left colon/rectum. CT enterography (CTE) showed multifocal asymmetric bowel wall thickening in distal ileum and TI and enlarged mesentery lymph nodes. He was started on steroids. Repeat CTE showed improvement in previously noted bowel wall thickening without pathologically enlarged lymph nodes. Given suspected CD, Ustekinumab was recommended, but the patient was admitted with exudative pleural effusion with negative cultures and cytology. CT chest with a nonspecific 5 mm nodule without mediastinal lymphadenopathy. PET scan showed mesenteric adenopathy and a right supraclavicular node with abnormal activity. Findings raised concerns for lymphoma. Repeat EGD showed deformed antrum/pylorus and nodular mucosa in duodenum (Figure 1); the previously seen duodenal ulcer had healed. Pathology revealed marginal zone MALT lymphoma with associated immunodeficiency. Bone marrow biopsy was negative. On Rituximab, PET scan showed large mesenteric masses raising suspicion for DLBCL. Mesenteric mass biopsy was scheduled, but he was admitted with sepsis and passed.
Discussion: Marginal zone MALT lymphoma is clinically an indolent form of lymphoma that can be misdiagnosed as CD and can occasionally progress to DLBCL. High index of suspicion is needed with low threshold for repeat endoscopy with biopsies in suspected cases.
References
1. Iwamuro M, Tanaka T, Okada H. Review of lymphoma in the duodenum: An update of diagnosis and management. World J Gastroenterol. 2023 Mar 28;29(12):1852-1862
Disclosures:
Anam Herekar, MD1, Menna Megahed, MD2, Harshitha Addagatla, MD3, Evangelos Tsipotis, MD3. P1020 - Extranodal Marginal Zone Lymphoma of Mucosa-Associated Lymphoid Tissue of the Stomach and Small Intestine Mimicking Crohn’s Disease With Suspected Transformation to Diffuse Large B-Cell Lymphoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Augusta University, Augusta, GA; 2Augusta, GA; 3Augusta University Medical Center, Augusta, GA
Introduction: Extranodal marginal zone mucosa-associated lymphoma (MALT), is a form of non-Hodgkin’s lymphoma most commonly found in stomach. (1) Rarely, it can be seen in the small intestine and can progress to Diffuse large B-cell lymphoma (DLBCL). (1) It can mimic Crohn’s Disease (CD) delaying diagnosis. We present a rare case of marginal zone MALT lymphoma mimicking CD with suspected transformation to DLBCL.
Case Description/Methods: 42-year-old male presented to gastroenterology clinic with weight loss, chronic lower extremity edema and diarrhea. Labs with albumin < 1.5 mg/dL elevated IgA with low IgG and IgM, Quantiferon negative, ESR 110 mm/hr and CRP 3.2 mg/dL, Calprotectin >800 ug/g, and low fecal elastase. Stool studies positive for EPEC/EAEC treated with azithromycin. Endoscopic evaluation showed nodular gastric and duodenal mucosa, a large duodenal bulb ulcer, nodular mucosa of the terminal ileum (TI) and rectal erythema. Pathology showed chronic gastritis, chronic active cryptitis in duodenum and TI, and chronic colitis in the left colon/rectum. CT enterography (CTE) showed multifocal asymmetric bowel wall thickening in distal ileum and TI and enlarged mesentery lymph nodes. He was started on steroids. Repeat CTE showed improvement in previously noted bowel wall thickening without pathologically enlarged lymph nodes. Given suspected CD, Ustekinumab was recommended, but the patient was admitted with exudative pleural effusion with negative cultures and cytology. CT chest with a nonspecific 5 mm nodule without mediastinal lymphadenopathy. PET scan showed mesenteric adenopathy and a right supraclavicular node with abnormal activity. Findings raised concerns for lymphoma. Repeat EGD showed deformed antrum/pylorus and nodular mucosa in duodenum (Figure 1); the previously seen duodenal ulcer had healed. Pathology revealed marginal zone MALT lymphoma with associated immunodeficiency. Bone marrow biopsy was negative. On Rituximab, PET scan showed large mesenteric masses raising suspicion for DLBCL. Mesenteric mass biopsy was scheduled, but he was admitted with sepsis and passed.
Discussion: Marginal zone MALT lymphoma is clinically an indolent form of lymphoma that can be misdiagnosed as CD and can occasionally progress to DLBCL. High index of suspicion is needed with low threshold for repeat endoscopy with biopsies in suspected cases.
References
1. Iwamuro M, Tanaka T, Okada H. Review of lymphoma in the duodenum: An update of diagnosis and management. World J Gastroenterol. 2023 Mar 28;29(12):1852-1862
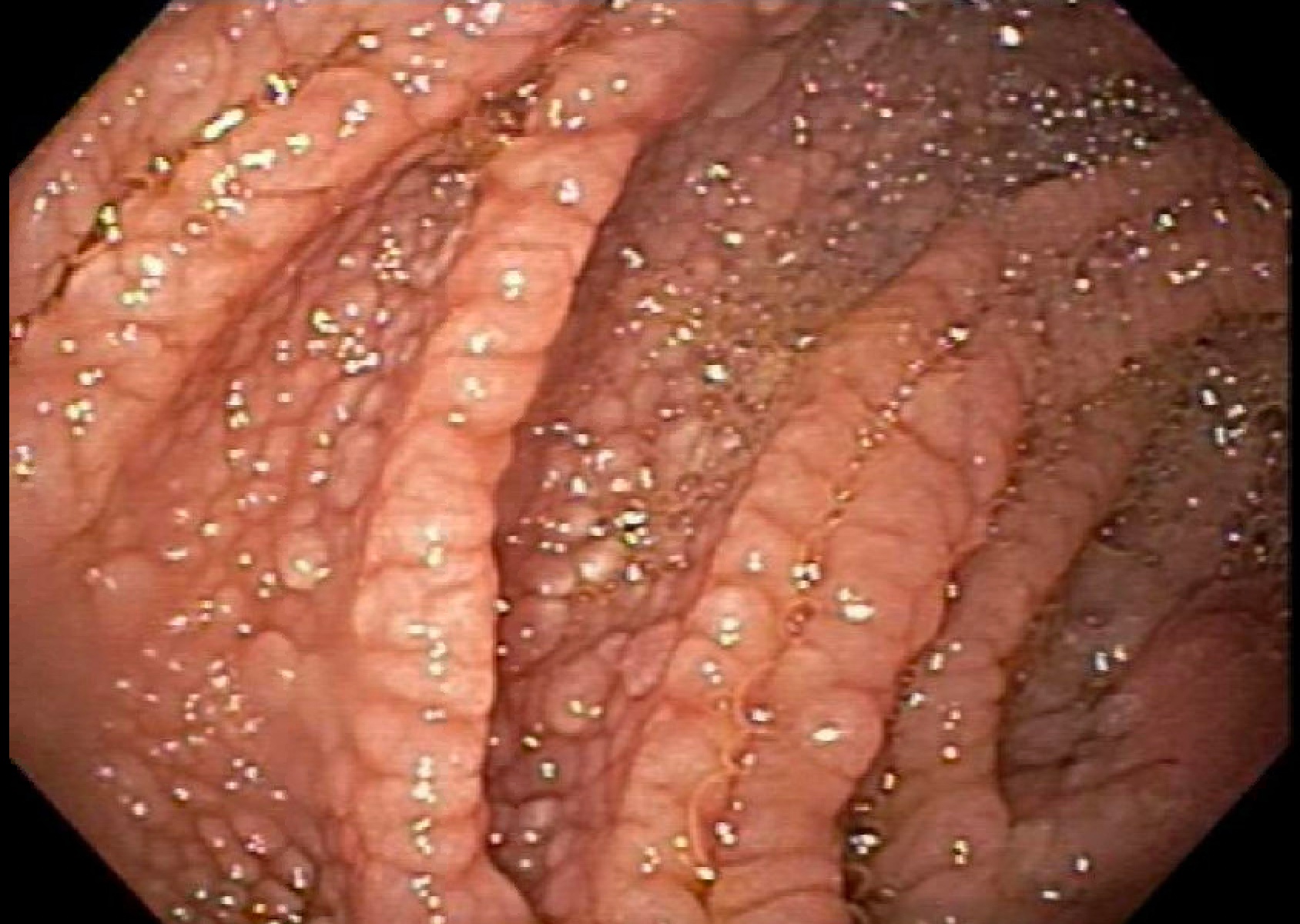
Figure: Fig 1. Nodular Duodenal Mucosa
Disclosures:
Anam Herekar indicated no relevant financial relationships.
Menna Megahed indicated no relevant financial relationships.
Harshitha Addagatla indicated no relevant financial relationships.
Evangelos Tsipotis indicated no relevant financial relationships.
Anam Herekar, MD1, Menna Megahed, MD2, Harshitha Addagatla, MD3, Evangelos Tsipotis, MD3. P1020 - Extranodal Marginal Zone Lymphoma of Mucosa-Associated Lymphoid Tissue of the Stomach and Small Intestine Mimicking Crohn’s Disease With Suspected Transformation to Diffuse Large B-Cell Lymphoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
