Sunday Poster Session
Category: Interventional Endoscopy
P1045 - Predictors of Readmission Following ERCP: A Five Year Nationwide Study in the United States
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Hayden E. Rotramel, MD
SSM Health St. Louis University Hospital
St. Louis, MO
Presenting Author(s)
Mahmoud Y. Madi, MD1, Yassine Kilani, MD1, Hayden Rotramel, MD2, Wissam Kiwan, MD3, Ahmad Najdat Bazarbashi, MD4
1SSM Health Saint Louis University Hospital, St. Louis, MO; 2SSM Health St. Louis University Hospital, St. Louis, MO; 3Saint Louis University, St. Louis, MO; 4Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, MO
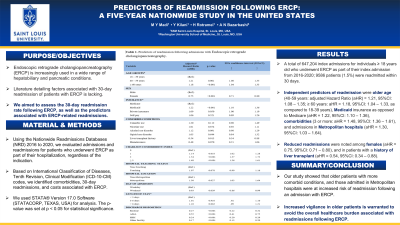
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) is increasingly used in a wide range of hepatobiliary and pancreatic conditions. Literature detailing factors associated with 30-day readmission of patients with ERCP is lacking. We aimed to assess the 30-day readmission rate following ERCP, as well as the predictors associated with ERCP-related readmissions.
Methods: Using the Nationwide Readmissions Databases (NRD) 2016 to 2020, we evaluated admissions and readmissions for patients who underwent ERCP as part of their hospitalization, regardless of the indication. On the basis of International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes, we identified comorbidities, 30-day readmissions, and costs associated with ERCP. We used STATA® Version 17.0 Software (STATACORP, TEXAS, USA) for analysis. The p-value was set at p < 0.05 for statistical significance.
Results: A total of 647,204 index admissions for individuals ≥ 18 years old who underwent ERCP as part of their index admission from 2016-2020; 9586 patients (1.5%) were readmitted within 30 days. Mortality was increased among readmissions (2.2%) as compared to index admissions (1.7%, p< 0.001). Readmissions following ERCP amounted to a mean cost of $82,557 and an average length of stay of 6 days. 8% of readmissions were attributed to acute pancreatitis. Independent predictors of readmission were age older age (40-59 years: adjusted Hazard Ratio (aHR) = 1.21, 95%CI: 1.08 – 1.35; ≥ 60 years: aHR = 1.18, 95%CI: 1.04 – 1.33, as compared to 18-39 years), Medicaid insurance as opposed to Medicare (aHR = 1.22, 95%CI: 1.10 – 1.36), comorbidities (3 or more: aHR = 1.48, 95%CI: 1.36 – 1.61), and admissions in Metropolitan hospitals (aHR = 1.30, 95%CI: 1.03 – 1.64). On the other hand, reduced readmissions were noted among females (aHR = 0.75, 95%CI: 0.71 – 0.80), and in patients with a history of liver transplant (aHR = 0.54, 95%CI: 0.34 – 0.88).
Discussion: Our study showed that older patients with more comorbid conditions, and those admitted in Metropolitan hospitals were at increased risk of readmission following an admission with ERCP. On the other hand, patients with a history of liver transplant were at reduced risk of readmission. Increased vigilance in older patients is warranted to avoid the overall healthcare burden associated with readmissions following ERCP.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mahmoud Y. Madi, MD1, Yassine Kilani, MD1, Hayden Rotramel, MD2, Wissam Kiwan, MD3, Ahmad Najdat Bazarbashi, MD4. P1045 - Predictors of Readmission Following ERCP: A Five Year Nationwide Study in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1SSM Health Saint Louis University Hospital, St. Louis, MO; 2SSM Health St. Louis University Hospital, St. Louis, MO; 3Saint Louis University, St. Louis, MO; 4Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, MO
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) is increasingly used in a wide range of hepatobiliary and pancreatic conditions. Literature detailing factors associated with 30-day readmission of patients with ERCP is lacking. We aimed to assess the 30-day readmission rate following ERCP, as well as the predictors associated with ERCP-related readmissions.
Methods: Using the Nationwide Readmissions Databases (NRD) 2016 to 2020, we evaluated admissions and readmissions for patients who underwent ERCP as part of their hospitalization, regardless of the indication. On the basis of International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes, we identified comorbidities, 30-day readmissions, and costs associated with ERCP. We used STATA® Version 17.0 Software (STATACORP, TEXAS, USA) for analysis. The p-value was set at p < 0.05 for statistical significance.
Results: A total of 647,204 index admissions for individuals ≥ 18 years old who underwent ERCP as part of their index admission from 2016-2020; 9586 patients (1.5%) were readmitted within 30 days. Mortality was increased among readmissions (2.2%) as compared to index admissions (1.7%, p< 0.001). Readmissions following ERCP amounted to a mean cost of $82,557 and an average length of stay of 6 days. 8% of readmissions were attributed to acute pancreatitis. Independent predictors of readmission were age older age (40-59 years: adjusted Hazard Ratio (aHR) = 1.21, 95%CI: 1.08 – 1.35; ≥ 60 years: aHR = 1.18, 95%CI: 1.04 – 1.33, as compared to 18-39 years), Medicaid insurance as opposed to Medicare (aHR = 1.22, 95%CI: 1.10 – 1.36), comorbidities (3 or more: aHR = 1.48, 95%CI: 1.36 – 1.61), and admissions in Metropolitan hospitals (aHR = 1.30, 95%CI: 1.03 – 1.64). On the other hand, reduced readmissions were noted among females (aHR = 0.75, 95%CI: 0.71 – 0.80), and in patients with a history of liver transplant (aHR = 0.54, 95%CI: 0.34 – 0.88).
Discussion: Our study showed that older patients with more comorbid conditions, and those admitted in Metropolitan hospitals were at increased risk of readmission following an admission with ERCP. On the other hand, patients with a history of liver transplant were at reduced risk of readmission. Increased vigilance in older patients is warranted to avoid the overall healthcare burden associated with readmissions following ERCP.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mahmoud Madi indicated no relevant financial relationships.
Yassine Kilani indicated no relevant financial relationships.
Hayden Rotramel indicated no relevant financial relationships.
Wissam Kiwan indicated no relevant financial relationships.
Ahmad Najdat Bazarbashi indicated no relevant financial relationships.
Mahmoud Y. Madi, MD1, Yassine Kilani, MD1, Hayden Rotramel, MD2, Wissam Kiwan, MD3, Ahmad Najdat Bazarbashi, MD4. P1045 - Predictors of Readmission Following ERCP: A Five Year Nationwide Study in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
