Sunday Poster Session
Category: Interventional Endoscopy
P1059 - Biliary Access Using Needle Knife Fistulotomy as an Initial Method of Cannulation in Patients With Average and High Risk of Post-ERCP Pancreatitis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

João Fernandes, MD
ULS Alto Minho; ICVS – Life and Health Sciences Research Institute and ICVS/3B’s; ULS Cova da Beira
Viseu, Viseu, Portugal
Presenting Author(s)
João Fernandes, MD1, Fábio Correia, MD2, Henrique Coelho, MD2, Rita Ribeiro, MD3, Alda Andrade, MD3, Isabel Tarrio, MD3, Tarcísio Araújo, MD3, Gonçalo Alexandrino, MD2, Luís Lourenço, MD4, David Horta, MD4, Patrício Costa, PhD5, Luís Lopes, MD, PhD, MBA6, Jorge Canena, MD, PhD4
1ULS Alto Minho; ICVS – Life and Health Sciences Research Institute and ICVS/3B’s; ULS Cova da Beira, Viseu, Viseu, Portugal; 2Amadora Sintra Hospital, Lisbon, Lisboa, Portugal; 3ULS Alto Minho, Viana do Castelo, Viana do Castelo, Portugal; 4University Department of Gastroenterology - CUF Tejo Hospital - Nova Medical School; Amadora Sinta Hospital, Lisbon, Lisboa, Portugal; 5ICVS – Life and Health Sciences Research Institute and ICVS/3B’s, Viana do Castelo, Viana do Castelo, Portugal; 6ULS Alto Minho; ICVS – Life and Health Sciences Research Institute and ICVS/3B’s, Viana do Castelo, Viana do Castelo, Portugal
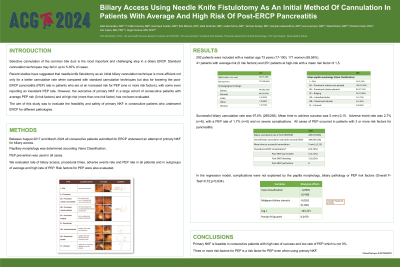
Introduction: Recent studies have suggested that needle-knife fistulotomy as an initial biliary cannulation technique is more efficient not only for a better cannulation rate when compared with standard cannulation techniques mas also for lowering the post-ERCP pancreatitis (PEP) rate in patients who are at an increased risk for PEP (one or more risk factors). However, the outcomes of primary NKF in a large cohort of consecutive patients with average PEP risk (0 risk factors) and at high risk (more than one risk factor) has not been evaluated.
Methods: All consecutive patients submitted to ERCP underwent an attempt of primary NKF for biliary access. Flat and diverticular papillae were excluded, and PEP prevention was used in all cases. We evaluated rate of biliary access, procedural times, adverse events rate and PEP rate in all patients and in subgroups of average and high rate of PEP. Risk factors for PEP were evaluated.
Results: 292 patients were included-41 patients with average risk and 251 patients at high-risk with a mean risk factor of 1,5. Successful biliary cannulation rate was 97,6% (285/292). Mean time to achieve success was 5 min+2,15. Adverse event rate was 2,7% (n=8), with a PEP rate of 1,7% (n=5) and no severe complications. All cases of PEP occurred in patients with 3 or more risk factors for pancreatitis (p< 0.001).
Discussion: Primary NKF is feasible in consecutive patients with high rate of success and low rate of PEP which is not 0%. Three or more risk-factors for PEP is a risk factor for PEP even when using primary NKF.
ClinicalTrials.gov ID NCT06452875
Disclosures:
João Fernandes, MD1, Fábio Correia, MD2, Henrique Coelho, MD2, Rita Ribeiro, MD3, Alda Andrade, MD3, Isabel Tarrio, MD3, Tarcísio Araújo, MD3, Gonçalo Alexandrino, MD2, Luís Lourenço, MD4, David Horta, MD4, Patrício Costa, PhD5, Luís Lopes, MD, PhD, MBA6, Jorge Canena, MD, PhD4. P1059 - Biliary Access Using Needle Knife Fistulotomy as an Initial Method of Cannulation in Patients With Average and High Risk of Post-ERCP Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1ULS Alto Minho; ICVS – Life and Health Sciences Research Institute and ICVS/3B’s; ULS Cova da Beira, Viseu, Viseu, Portugal; 2Amadora Sintra Hospital, Lisbon, Lisboa, Portugal; 3ULS Alto Minho, Viana do Castelo, Viana do Castelo, Portugal; 4University Department of Gastroenterology - CUF Tejo Hospital - Nova Medical School; Amadora Sinta Hospital, Lisbon, Lisboa, Portugal; 5ICVS – Life and Health Sciences Research Institute and ICVS/3B’s, Viana do Castelo, Viana do Castelo, Portugal; 6ULS Alto Minho; ICVS – Life and Health Sciences Research Institute and ICVS/3B’s, Viana do Castelo, Viana do Castelo, Portugal
Introduction: Recent studies have suggested that needle-knife fistulotomy as an initial biliary cannulation technique is more efficient not only for a better cannulation rate when compared with standard cannulation techniques mas also for lowering the post-ERCP pancreatitis (PEP) rate in patients who are at an increased risk for PEP (one or more risk factors). However, the outcomes of primary NKF in a large cohort of consecutive patients with average PEP risk (0 risk factors) and at high risk (more than one risk factor) has not been evaluated.
Methods: All consecutive patients submitted to ERCP underwent an attempt of primary NKF for biliary access. Flat and diverticular papillae were excluded, and PEP prevention was used in all cases. We evaluated rate of biliary access, procedural times, adverse events rate and PEP rate in all patients and in subgroups of average and high rate of PEP. Risk factors for PEP were evaluated.
Results: 292 patients were included-41 patients with average risk and 251 patients at high-risk with a mean risk factor of 1,5. Successful biliary cannulation rate was 97,6% (285/292). Mean time to achieve success was 5 min+2,15. Adverse event rate was 2,7% (n=8), with a PEP rate of 1,7% (n=5) and no severe complications. All cases of PEP occurred in patients with 3 or more risk factors for pancreatitis (p< 0.001).
Discussion: Primary NKF is feasible in consecutive patients with high rate of success and low rate of PEP which is not 0%. Three or more risk-factors for PEP is a risk factor for PEP even when using primary NKF.
ClinicalTrials.gov ID NCT06452875
Disclosures:
João Fernandes indicated no relevant financial relationships.
Fábio Correia indicated no relevant financial relationships.
Henrique Coelho indicated no relevant financial relationships.
Rita Ribeiro indicated no relevant financial relationships.
Alda Andrade indicated no relevant financial relationships.
Isabel Tarrio indicated no relevant financial relationships.
Tarcísio Araújo indicated no relevant financial relationships.
Gonçalo Alexandrino indicated no relevant financial relationships.
Luís Lourenço indicated no relevant financial relationships.
David Horta indicated no relevant financial relationships.
Patrício Costa indicated no relevant financial relationships.
Luís Lopes indicated no relevant financial relationships.
Jorge Canena indicated no relevant financial relationships.
João Fernandes, MD1, Fábio Correia, MD2, Henrique Coelho, MD2, Rita Ribeiro, MD3, Alda Andrade, MD3, Isabel Tarrio, MD3, Tarcísio Araújo, MD3, Gonçalo Alexandrino, MD2, Luís Lourenço, MD4, David Horta, MD4, Patrício Costa, PhD5, Luís Lopes, MD, PhD, MBA6, Jorge Canena, MD, PhD4. P1059 - Biliary Access Using Needle Knife Fistulotomy as an Initial Method of Cannulation in Patients With Average and High Risk of Post-ERCP Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
