Sunday Poster Session
Category: Interventional Endoscopy
P1104 - Sugar Shortage: A Case of Insulinoma Managed by EUS-Guided Ethanol Ablation
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Rachel Moffett, DO
Carolinas Medical Center Internal Medicine Residency
Charlotte, NC
Presenting Author(s)
Award: Presidential Poster Award
Rachel Moffett, DO1, Mary Alexandra Bramlage, MD2, Andrew Dries, MD3
1Carolinas Medical Center Internal Medicine Residency, Charlotte, NC; 2University of Florida, Ponce Inlet, FL; 3Atrium Health, Charlotte, NC
Introduction: Pancreatic neuroendocrine tumors (PNET) are uncommon neoplasms, and roughly half cause symptoms related to excess hormone production. If the tumor secretes insulin, it is termed an insulinoma and leads to recurrent severe hypoglycemia. Diagnosis can be challenging due to episodic and variable symptoms and small tumor size. Surgical resection is generally curative however may carry notable risk in patients with multiple comorbidities. Endoscopic ultrasound (EUS) with ethanol ablation is an alternative treatment.
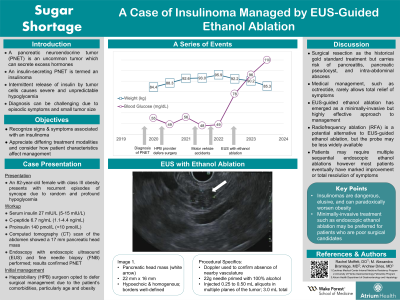
Case Description/Methods: An 82-year-old female with morbid obesity presented with recurrent episodes of syncope due to hypoglycemia. Additional endocrine studies revealed elevated serum insulin, C-peptide, and proinsulin as well as a negative sulfonylurea screen, collectively suggestive of insulinoma. Computed tomography (CT) scan of the abdomen showed a 17 mm pancreatic head mass. Endoscopy with EUS and fine needle biopsy (FNB) were performed, and pathology confirmed PNET. The patient was seen by a hepatobiliary surgeon who opted to defer surgical management due to the patient's advanced age and additional comorbidities. Unfortunately, continued hypoglycemic episodes led to multiple car accidents. The patient then underwent EUS-guided ethanol ablation; a total of 3.0 mL of 100% alcohol were injected in 0.25-0.50 mL aliquots in multiple planes of the tumor. In the following year, she had rapid improvement in her serum blood glucose without further hypoglycemia, and she was able to lose nearly 20 lbs.
Discussion: Historically, surgical resection has been the gold standard for insulinoma treatment but does carry risk of pancreatitis, pancreatic pseudocyst, or intra-abdominal abscess. For patients who are unwilling or unable to undergo surgery, medical management is another option but is rarely sufficient to fully control symptoms. Fortunately, EUS-guided ethanol ablation has emerged as a less-invasive but highly effective alternative approach. Some patients may require multiple procedures in sequence however the majority of patients eventually have marked improvement or total resolution of hypoglycemia-related symptoms following ethanol ablation. Additional head-to-head studies comparing ethanol ablation and surgical management are needed, but an endoscopic approach may be better tolerated, particularly for patients who are poor surgical candidates.

Disclosures:
Rachel Moffett, DO1, Mary Alexandra Bramlage, MD2, Andrew Dries, MD3. P1104 - Sugar Shortage: A Case of Insulinoma Managed by EUS-Guided Ethanol Ablation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Rachel Moffett, DO1, Mary Alexandra Bramlage, MD2, Andrew Dries, MD3
1Carolinas Medical Center Internal Medicine Residency, Charlotte, NC; 2University of Florida, Ponce Inlet, FL; 3Atrium Health, Charlotte, NC
Introduction: Pancreatic neuroendocrine tumors (PNET) are uncommon neoplasms, and roughly half cause symptoms related to excess hormone production. If the tumor secretes insulin, it is termed an insulinoma and leads to recurrent severe hypoglycemia. Diagnosis can be challenging due to episodic and variable symptoms and small tumor size. Surgical resection is generally curative however may carry notable risk in patients with multiple comorbidities. Endoscopic ultrasound (EUS) with ethanol ablation is an alternative treatment.
Case Description/Methods: An 82-year-old female with morbid obesity presented with recurrent episodes of syncope due to hypoglycemia. Additional endocrine studies revealed elevated serum insulin, C-peptide, and proinsulin as well as a negative sulfonylurea screen, collectively suggestive of insulinoma. Computed tomography (CT) scan of the abdomen showed a 17 mm pancreatic head mass. Endoscopy with EUS and fine needle biopsy (FNB) were performed, and pathology confirmed PNET. The patient was seen by a hepatobiliary surgeon who opted to defer surgical management due to the patient's advanced age and additional comorbidities. Unfortunately, continued hypoglycemic episodes led to multiple car accidents. The patient then underwent EUS-guided ethanol ablation; a total of 3.0 mL of 100% alcohol were injected in 0.25-0.50 mL aliquots in multiple planes of the tumor. In the following year, she had rapid improvement in her serum blood glucose without further hypoglycemia, and she was able to lose nearly 20 lbs.
Discussion: Historically, surgical resection has been the gold standard for insulinoma treatment but does carry risk of pancreatitis, pancreatic pseudocyst, or intra-abdominal abscess. For patients who are unwilling or unable to undergo surgery, medical management is another option but is rarely sufficient to fully control symptoms. Fortunately, EUS-guided ethanol ablation has emerged as a less-invasive but highly effective alternative approach. Some patients may require multiple procedures in sequence however the majority of patients eventually have marked improvement or total resolution of hypoglycemia-related symptoms following ethanol ablation. Additional head-to-head studies comparing ethanol ablation and surgical management are needed, but an endoscopic approach may be better tolerated, particularly for patients who are poor surgical candidates.

Figure: Pancreatic head mass (17 mm) noted on EUS.
Disclosures:
Rachel Moffett indicated no relevant financial relationships.
Mary Alexandra Bramlage indicated no relevant financial relationships.
Andrew Dries indicated no relevant financial relationships.
Rachel Moffett, DO1, Mary Alexandra Bramlage, MD2, Andrew Dries, MD3. P1104 - Sugar Shortage: A Case of Insulinoma Managed by EUS-Guided Ethanol Ablation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

